All fungal infections require antifungal medication for complete cure. While some infections are minor and may increase or decrease in intensity without medication, deep fungal infections can be fatal. Treatment for fungal infections varies greatly and while most can be cured by the application of local applications, others may even require surgery. An appropriate diagnosis is necessary for accurate treatment, and no medication should be taken without the advice of a doctor.
Some common treatment options for fungal infections are as follows:
Antifungal medicines
Antifungal medicines are topical, oral, or injectable medicines depending upon the type and severity of the infection. Antifungal medicines act by destroying the cell walls of the fungi, causing the cells to die. They also act by preventing the reproduction and the growth of fungi. There is a wide variety of antifungal agents available in the market belonging to different classes, such as polyene, tubulin disrupter, azoles, allylamine, a pyrimidine analog, and echinocandin.
Corticosteroids
Corticosteroids or steroids have been used to treat diseases since the end of the 1950s.
Some topical corticosteroids for skin are hydrocortisone, betamethasone, clobetasol, clobetasone/clobetasol, diflucortolone, and fluocinolone.
Oral corticosteroids include prednisolone, prednisone, methylprednisolone, dexamethasone, and hydrocortisone.
Injectable intravenous or intramuscular steroids include hydrocortisone, methylprednisolone, and dexamethasone. Inhaled corticosteroids include formulations, such as beclomethasone, fluticasone, budesonide, mometasone, and ciclesonide.
Embolisation of the Bronchial Artery
Haemoptysis, a condition wherein the patient is coughing blood, is treated through embolization of the bronchial artery in cases of a very severe fungal infection. The condition can range from mild to severe. Mild cases are treated with oral medicines, while severe cases may require hospitalization along with blood transfusion. Severe cases are difficult to treat and are often unpredictable. Rapid and frequent intervention and diagnosis are often required to control the various side-effects and prognosis of the condition.
Immunotherapy
In cases of invasive fungal infections, the immune system of the patient is severely compromised. Despite the availability of a wide range of antibiotics, death rates are very high at around 40%. Immunotherapy aims to fight invasive fungal infections by improving patients’ immune system.
- White blood cell (WBC) transfusion
These may help to improve the immunity of the patient and help fight infection. However, the quality of WBC transfused is critical. These transfusions help control the progression of severe infections that are not easily controlled by antibiotics.
- Granulocyte colony-stimulating factor
This therapy aims to stimulate the production of WBCs by the bone marrow and influences other parts of the immune system.
- Gamma interferon
Gamma interferon enhances the mechanism of immune cells and makes them better destroyers of fungi.
Surgery
Surgery may be required in severe cases of fungal infections where other treatment options have failed.
Brain
- Granuloma or cyptococcoma
Patients may need to undergo surgical removal of the infectious mass, especially if the mass is thought to be malignant. In patients who have had long periods of antifungal therapy, the organism may be in a static phase and further therapy may not help; in such cases, surgical removal is recommended.
- Cerebral abscess
Stereotactic drainage or complete removal of the abscess may be required depending on the position of the abscess.
Eye
- Endophthalmitis
A vitrectomy is advised for most cases of fungal endophthalmitis to remove the microbes and the debris.
- Keratitis
A surgery is generally advised to treat this condition especially when deep corneal lesions are present, as more than 50% of the patients do not respond positively to antifungal therapy.
Nose
In cases of chronic sinusitis, surgery removes all allergic mucin, fungal debris, and nasal polyps and preserves the underlying mucosa.
- Fungal ball of the sinuses
Surgical removal of the fungal ball has a high rate of curing the disease. Occasionally, an antifungal therapy may be also given to prevent local invasion.
Ear
Fungal infections of the ear often require surgical removal of the damaged tissue right up to the bone and may result in a complete hearing loss on the infected side.
Lungs
- Invasive pulmonary aspergillosis
An emergency surgery is often required to save the life, as the arteries are at a risk of a hemorrhage.
- Aspergilloma and chronic pulmonary aspergillosis
A surgery offers a high survival rate and prevents progression of the disease and further complications.
Heart
- Pericarditis
In case of a pericardial constriction, pericardiectomy or removal of a part of the pericardium may be required. Drainage may be initially required to control the infection after which a surgery may be conducted.
- Endocarditis infections
Surgery is one of the best treatment options for this infection and is conducted as early as possible. Recovery is generally difficult after complications arise.
- Pacemaker and cardioverter-defibrillator wire infection: In this case, lead-extraction needs to be undertaken along with sternotomy and a cardiopulmonary bypass surgery.
Bone
- Sternal wound infection
In this case, a surgery is conducted for debridement and for removal of wires in the infected area. The surgery is followed by an antifungal therapy.
- Vertebral body infection
This infection of the bones requires a surgery to remove the debris. Bone grafting may be required depending on the condition.
Lifestyle Management
Certain lifestyles make a person more prone to environmental pathogens, including fungi. If you are frequently infected by fungal infections and the cause is related to your work, such as gardening or tattooing, then a change of occupation may provide a solution. Doctors frequently advice people with recurring allergies to relocate to places with a more suitable climate. Although lifestyle does not play a major role in fungal infections, lifestyle management might help avoid recurring allergic infections.

 Doctors for Fungal Infections
Doctors for Fungal Infections  OTC Medicines for Fungal Infections
OTC Medicines for Fungal Infections
 Lab tests for Fungal Infections
Lab tests for Fungal Infections Fungal Infections articles
Fungal Infections articles
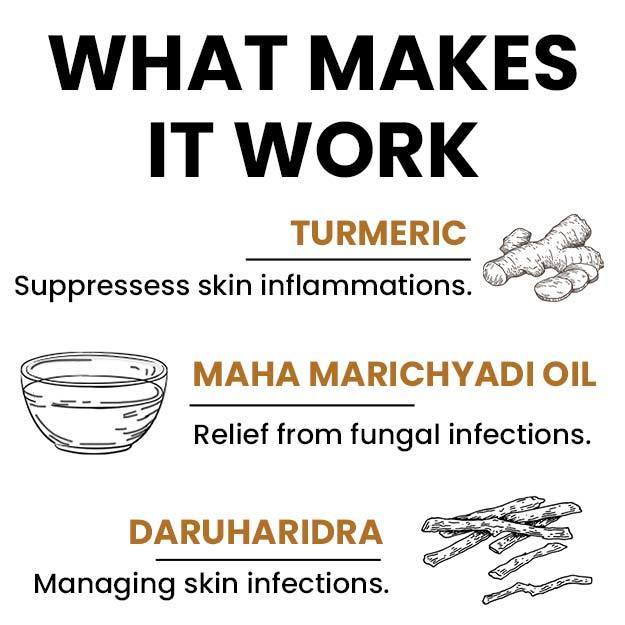
 Ayurvedic Treatment of Fungal Infections
Ayurvedic Treatment of Fungal Infections
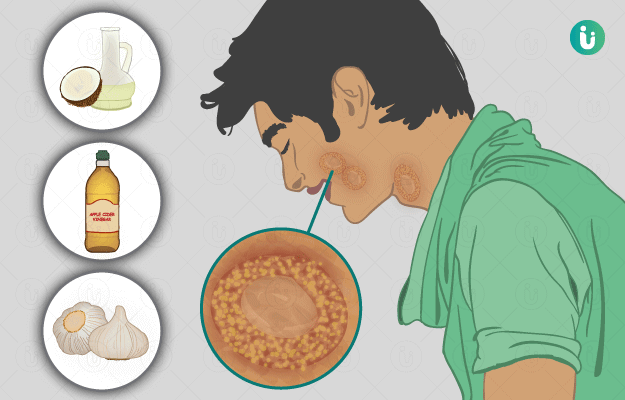
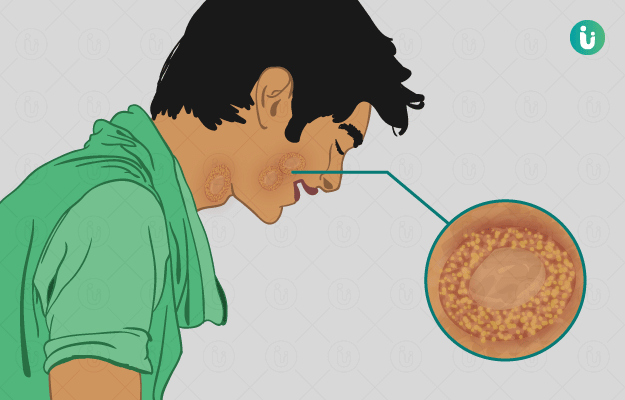
 Home Remedies for Fungal Infections
Home Remedies for Fungal Infections
 Homeopathic Treatment of Fungal Infections
Homeopathic Treatment of Fungal Infections
 Yoga for Fungal Infections
Yoga for Fungal Infections


























 Editorial Team
Editorial Team



 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla