Summary
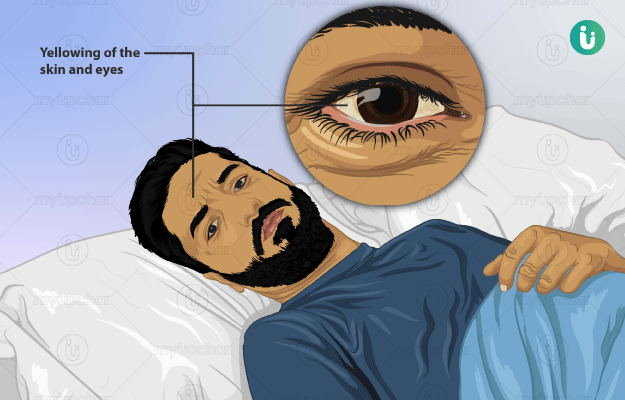
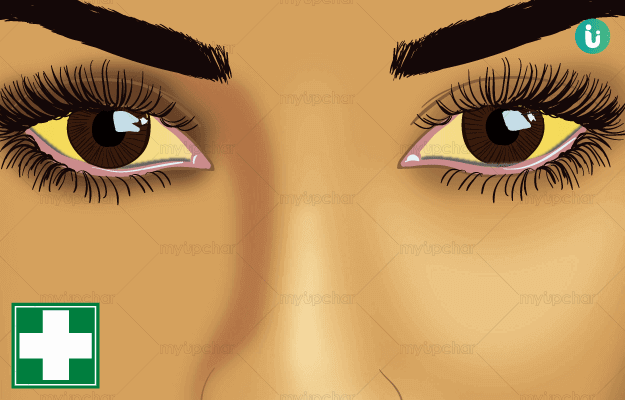
Jaundice is a disease in which the total serum bilirubin (TSB) level rises above 3 mg/dL. The symptoms include yellowing of your skin, the white part of your eyes, and mucous membranes (linings of internal soft organs such as mouth). Newborn babies usually have jaundice, but adults can suffer from it too. In adults, other symptoms are also seen such as stomach pain, loss of appetite, weight loss, etc. In babies, phototherapy and blood transfusion, while in adults, it includes removal of the causative factor, medications and sometimes, a surgery. If left untreated, it can affect the brain of the child, and other complications like sepsis, liver and kidney diseases or failure.
Metabolism of bilirubin
Our body keeps generating new red blood cells (RBCs) and wards off the old ones. During this process, the haemoglobin which is inside the old RBCs is broken down into globin, iron, and biliverdin. Globin and iron are re-utilised in our bone marrow to produce new haemoglobin, whereas biliverdin is broken down again to leave a byproduct called bilirubin. Our liver takes up this bilirubin for its further metabolism. This processed bilirubin flows through the bile duct and enters the intestine. The intestine also splits it down into urobilinogen and stercobilinogen. Urobilinogen is absorbed back again to be released into the blood circulation, some of which re-enters our liver while the rest of it is removed by our kidneys in the urine. Stercobilinogen is excreted out through stools.
Are you also troubled by obesity and are not able to lose weight even after a lot of efforts, then start using myUpchar Ayurveda Medarodh Weight Control Tablet today and control your weight.

 Doctors for Jaundice
Doctors for Jaundice  OTC Medicines for Jaundice
OTC Medicines for Jaundice
 Lab tests for Jaundice
Lab tests for Jaundice Jaundice articles
Jaundice articles
 Ayurvedic Treatment of Jaundice
Ayurvedic Treatment of Jaundice
 First Aid for Jaundice
First Aid for Jaundice
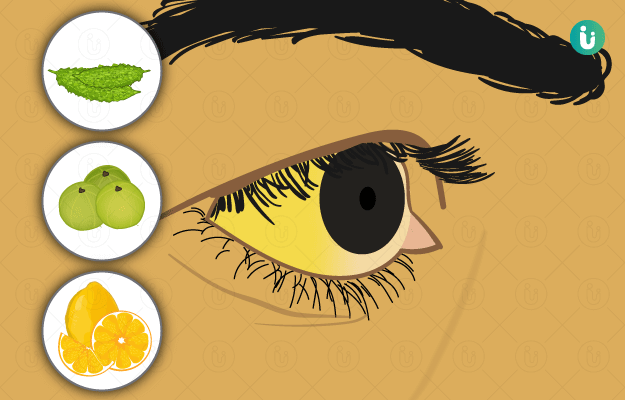
 Home Remedies for Jaundice
Home Remedies for Jaundice
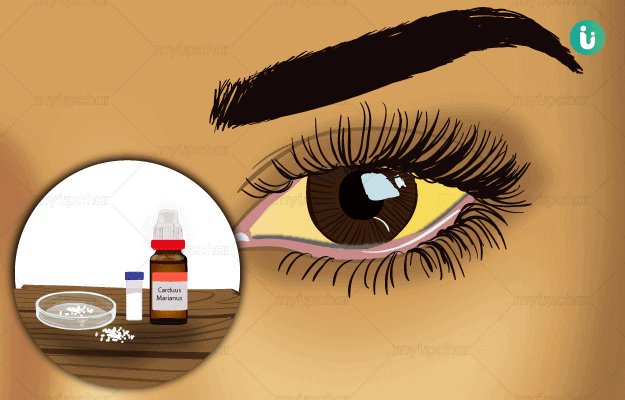
 Homeopathic Treatment of Jaundice
Homeopathic Treatment of Jaundice














 Editorial Team
Editorial Team

 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla

 Dt. Akanksha Mishra
Dt. Akanksha Mishra
 Dr. Rachita Narsaria
Dr. Rachita Narsaria











