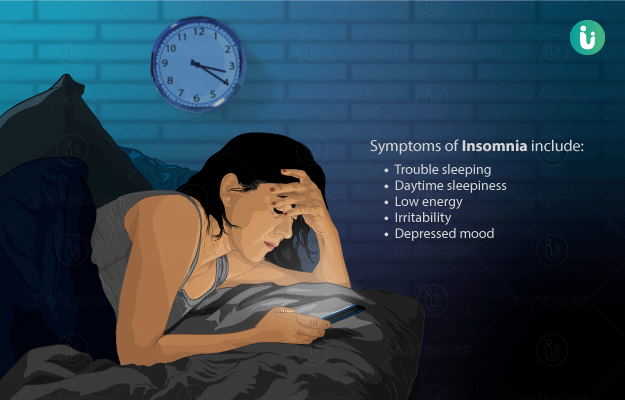
Adjustment insomnia
This type is also called as acute insomnia or short-term insomnia, disturbs your sleep and usually occurs because of stress. The sleep problem ends when the source of stress is gone or when you adapt to the stress. The stress does not always come from a negative experience. It has been observed that even something positive can make you too excited and not sleep well.
(Read More - Sleep problems in children)
Behavioural insomnia in children
This condition occurs when children don't go to bed on time unless a parent or guardian enforces a bedtime. If the children are made to go to bed at a specified time, then they tend to fall asleep at a normal hour. If they are not given strict bedtimes, then they may linger awake for hours at night.
(Read More - Sleep and mental health)
Idiopathic insomnia
Idiopathic insomnia is a lifelong sleep disorder that starts during infancy or childhood and continues into adulthood. This insomnia cannot be explained by other causes. It is not a result of any of the following.
- Other sleep disorders
- Medical problems
- Psychiatric disorders
- Stressful events
- Medication use
- Other behaviors
It may result from an imbalance in your body, such as an overactive awakening system and/or an underactive sleep system, but the true cause of this disorder is still unclear. Insomnia due to a drug or substance. This type of insomnia is directly related to the use of any of the following substances:
Your sleep is disrupted by your use of the any of the above substances. It may come as a surprise to you but this type of sleep problem may also occur when you stop using a substance.
Insomnia due to a medical condition
This type of insomnia is caused as a result of certain mental health disorders. Insomnia is a symptom of mental disorders. The course and severity of insomnia are directly linked to that of the mental health disorder, but this particular type of insomnia is a separate focus of treatment. This insomnia is a disorder only if it is severe enough to require separate treatment.
(Read More - Sleep chart)
Insomnia nonorganic, unspecified
This type of insomnia suggests that known substances and other physical causes of insomnia have been ruled out. This means that the cause of insomnia is most likely due to an underlying mental health disorder, psychological factor, or sleep-disruptive behaviours. This particular type may be predicted by doctors on a temporary basis while further evaluation and testing are being conducted. It is the name unspecified used when a person with insomnia does not meet the criteria for another type of insomnia.
Insomnia organic, unspecified
This type of insomnia is caused by a medical disorder, physical condition, or substance exposure. But the specific cause remains unclear. Further testing is required to discover the exact cause. The name may be used on a temporary basis while further evaluation and testing are completed.
(Read More - Home remedies for deep sleep)
Paradoxical insomnia
Paradoxical insomnia is a complaint of severe insomnia. It occurs without objective evidence of any sleep disturbance. Daytime side effects of insomnia vary in severity, but they tend to be far less severe than one would expect given the state of the condition. People with this disorder often report little or no sleep for one or more nights. They also describe having an intense awareness of the external environment or internal processes consistent with being awake. This awareness suggests a state of hyperarousal. A key feature which can be highlighted is an overestimation of the time it takes them to fall asleep. They also underestimate their total sleep time.
Psychophysiological insomnia
This type of insomnia is associated with excessive worrying, specifically focused on not being able to sleep. Insomnia may begin suddenly following an event or develop slowly over many years.
People with this sleep disorder worry too much about their insomnia and about being tired the next day. As a result, they learn to become tense and anxious as bedtime approaches. They may have racing thoughts that all relate to insomnia and trying to fall asleep. As they worry about falling asleep, they become more and tenser, which makes it less likely that they will be able to fall asleep
(Read More - Ways to overcome insomnia)

 Doctors for Insomnia
Doctors for Insomnia  OTC Medicines for Insomnia
OTC Medicines for Insomnia
 Lab tests for Insomnia
Lab tests for Insomnia Insomnia articles
Insomnia articles News for Insomnia
News for Insomnia
 Ayurvedic Treatment of Insomnia
Ayurvedic Treatment of Insomnia
 Homeopathic Treatment of Insomnia
Homeopathic Treatment of Insomnia












 Editorial Team
Editorial Team

 Dr. Ayush Pandey
Dr. Ayush Pandey


 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla


 Dt. Akanksha Mishra
Dt. Akanksha Mishra











