Several risk factors have been associated with a miscarried foetus. These include older age, obesity, and lifestyle habits like alcohol and smoking. However, the woman is generally not responsible for it.
Let us look at some of the evidence-based factors that are responsible for miscarriage in the first and second trimester.
Chromosomal abnormalities
A baby receives half of its DNA from each parent, therefore, any abnormality in parental chromosomal structure can be transferred to the foetus. An abnormal karyotype (chromosomal structure) in the foetus is one of the most common reasons for early and repeated miscarriages. However, studies suggest that couples who carry such abnormalities are equally viable of normal pregnancy as non-career couples even though they have a higher chance of miscarriage.
(Read more: Karyotype test)
Also, there are chromosomal tests that can determine if the parents carry such an abnormality in their DNA. You can get medical counselling about the best way to conceive in such conditions. Even though these are a bit costly, a DNA analysis is usually advised in case of recurrent miscarriages. So, this is definitely not something to worry about.
Usually, preimplantation genetic diagnosis (PGD) is believed to increase the chances of a live birth but the evidence is insufficient. In vitro fertilisation may also be a way to conceive in such cases.
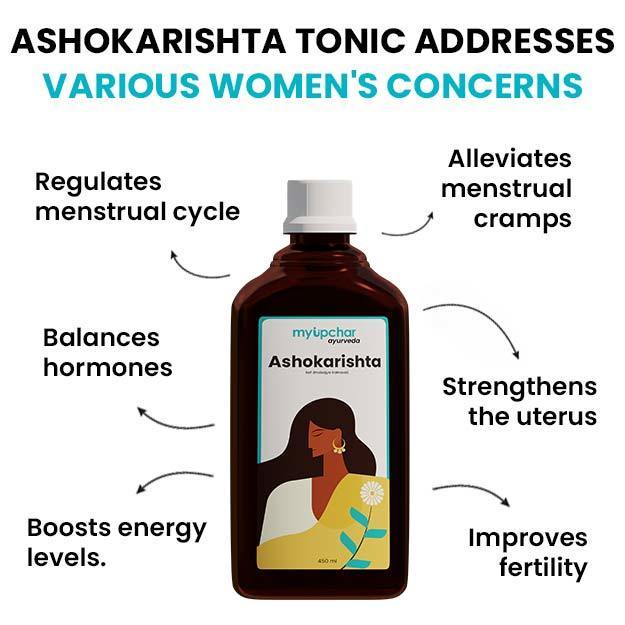
Thyroid dysfunction
An increased level of Human chorionic gonadotropin (HCG) has effects on various thyroid hormones. While the condition is reversible and non-harmful in most women, it might pose a threat of miscarriage and stillbirths in women who already have hormonal abnormalities. According to a study, normal but elevated levels of TSH levels, >2.5 mlU/L increase the risk of miscarriage.
(Read more: Thyroid problems during pregnancy)
The same goes for women with thyroid autoimmunity (when the body makes antibodies against the thyroid gland). One belief is that a higher number of autoantibodies delays conception and stimulates the immune system, in general, leading to spontaneous loss of the foetus. However, it was found to be independent of thyroid autoantibody titer.
(Read more: How to get pregnant with thyroid problems)
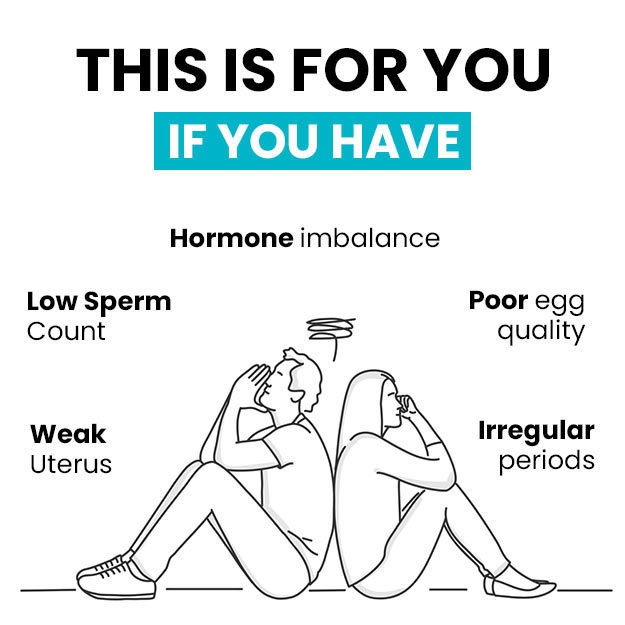
PCOS or polycystic ovary syndrome
PCOS is yet another hormonal imbalance that has been found to be responsible for early pregnancy loss. Extensive research has been done to understand the underlying mechanism behind this condition. However, the evidence is inconclusive. A number of factors are associated with PCOS related miscarriage. These include:
- Obesity
- Abnormal luteinizing hormone
- Increased insulin resistance
- Endometrial dysfunction
- Increased blood clotting in placenta
Immune dysfunction
While the maternal immune system is known to support implantation, there is controversial evidence that dysfunction in the mother’s immune system may terminate a pregnancy. On a general note, autoantibodies have been associated with an increased risk of recurrent miscarriage. Animal studies link the absence of certain immunological molecules to foetal loss.
According to a study published in Human reproduction, miscarrying women have an increased TNF level and Inflammation. In a previous study, imbalances in NK (natural killer) cells activation and function are claimed to be responsible for early termination of pregnancy.
Thrombophilia
Thrombophilia refers to a condition wherein the body is predisposed to increased blood clotting. It can either be genetic or acquired. Studies suggest that women who suffer from thrombophilia are at a higher risk of miscarriage due to clot formation and restriction of blood flow to the placenta. Clinical studies demonstrate that using low doses of anti-clotting medicines may increase the chances of foetal survival in these women. However, the evidence is not that strong. So, if you are suffering from thrombophilia, it is strongly recommended that you talk to your doctor instead of self-medicating.
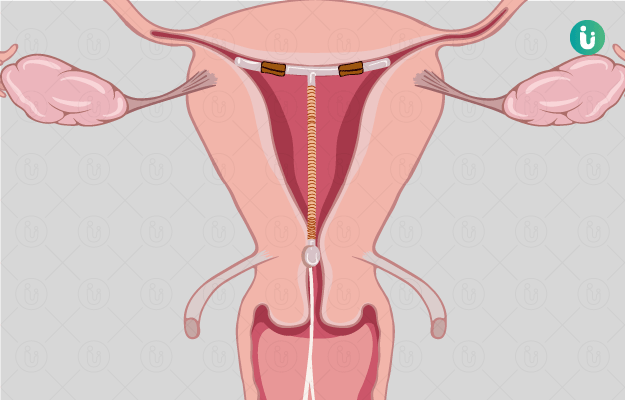
Ectopic pregnancy
Ectopic pregnancy happens when the embryo implants itself inside the fallopian tube. Since the fallopian tube cannot extend beyond a particular size, this type of pregnancy either terminates or needs to be removed as it can pose a serious threat to the mother. Statistics suggest that one in four ectopic pregnancies turn into a miscarriage.
Some of the common symptoms of ectopic pregnancy include:
If you notice any of these signs, it is advisable that you immediately consult your doctor.
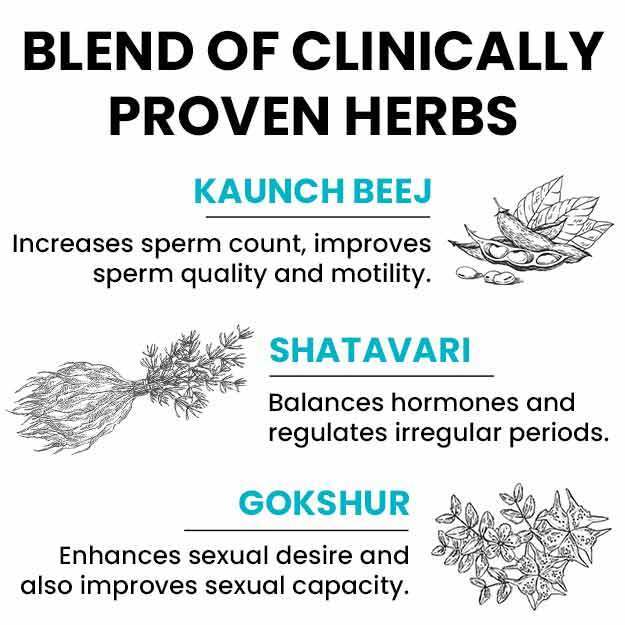
Sperm DNA fragmentation
A number of studies have been done to assess the effects of fragmented sperm DNA on the ease of conceiving. The results aren’t without contradiction. However, a study published in the ARC Journal of Gynaecology and obstetrics suggests that a higher level of sperm DNA damage is associated with an increased risk of miscarriage especially in case of recurrent pregnancy loss.
(Read more: Sperm DNA fragmentation test)
Other reasons for miscarriage
Apart from the above factors, miscarriage may also be caused due to:
What does not cause miscarriage in healthy women