Summary
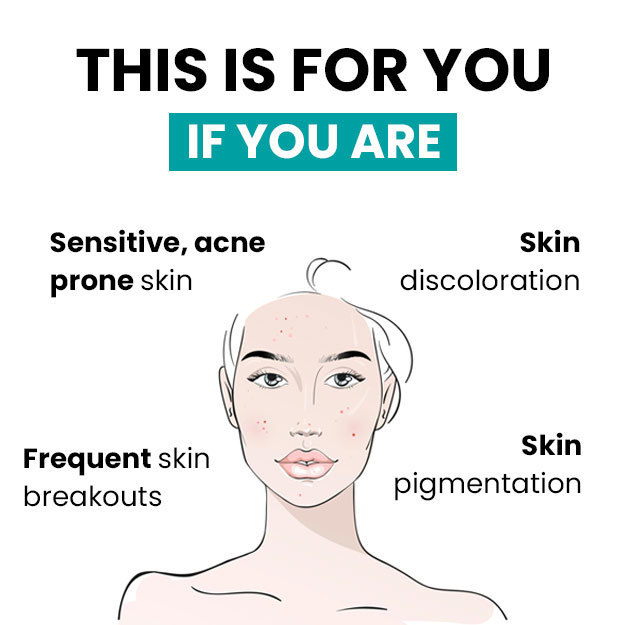
Psoriasis is a chronic skin condition triggered by an abnormal multiplication of cells of the skin. These skin cells multiply rapidly and trigger swelling of the affected area. Psoriasis usually causes red patches over the skin. The red patches cause soreness and are covered with terribly itchy silvery-white scales. The physiological symptoms show several phases of waxing and waning, but unfortunately, there is no cure for this disease. However, with adequate therapy, symptoms can be kept under control. Targeted therapy (local application, phototherapy and oral medications) along with lifestyle changes (such as avoiding stress, using moisturizers, avoiding smoking and alcohol consumption) usually prolongs the period of remission (symptom-free phase).

 Doctors for Psoriasis
Doctors for Psoriasis  OTC Medicines for Psoriasis
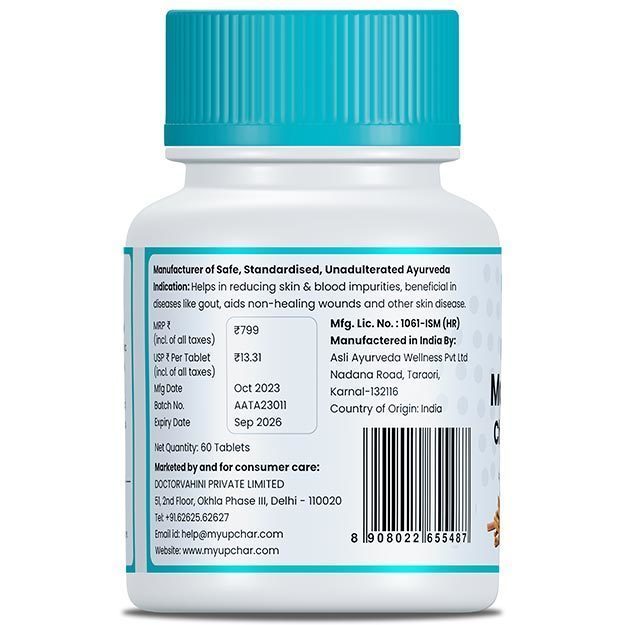
OTC Medicines for Psoriasis
 Psoriasis articles
Psoriasis articles News for Psoriasis
News for Psoriasis

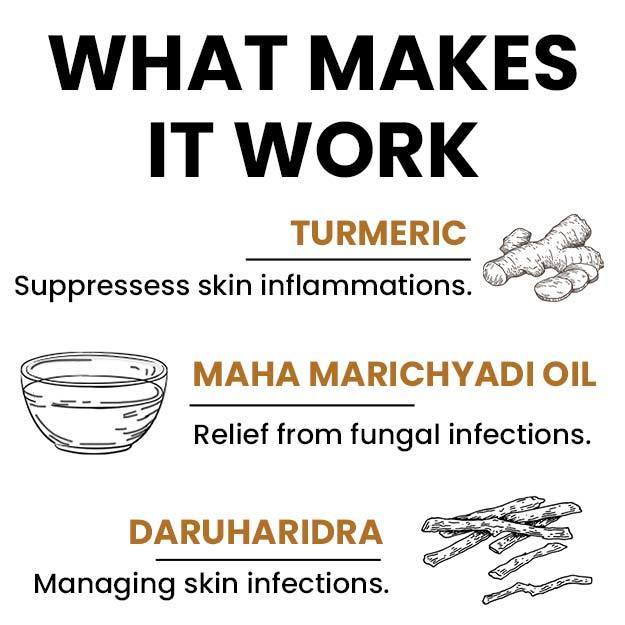
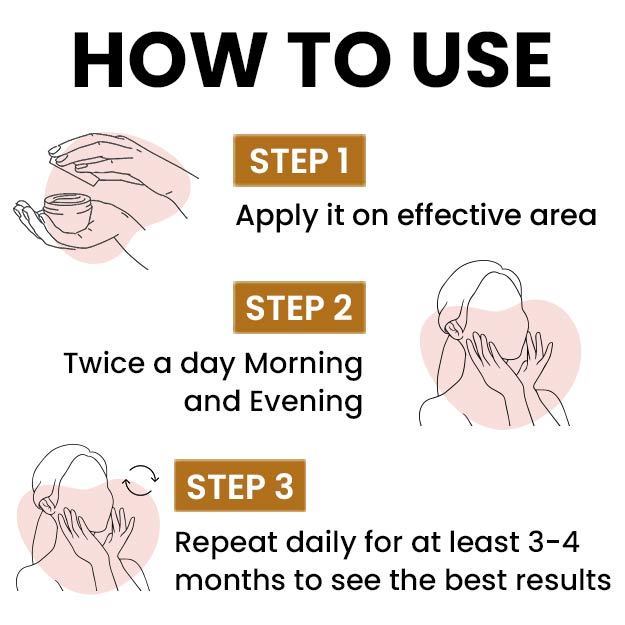
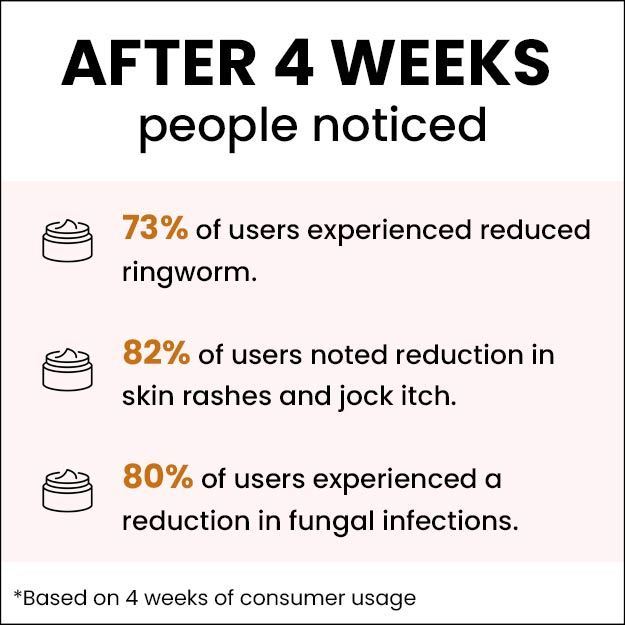
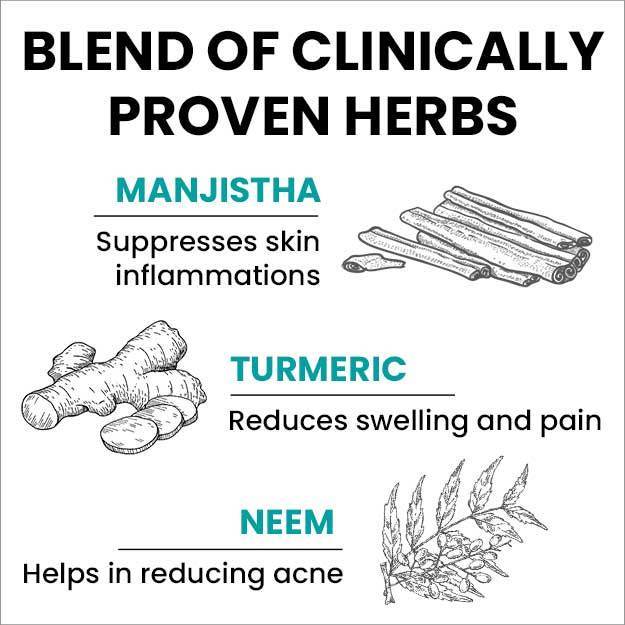
 Ayurvedic Treatment of Psoriasis
Ayurvedic Treatment of Psoriasis
 Diet for Psoriasis
Diet for Psoriasis
 Home Remedies for Psoriasis
Home Remedies for Psoriasis
 Homeopathic Treatment of Psoriasis
Homeopathic Treatment of Psoriasis




























 Editorial Team
Editorial Team

 Dr. Apratim Goel
Dr. Apratim Goel


 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla

 Dt. Akanksha Mishra
Dt. Akanksha Mishra












