Every woman wishes for a pregnancy that is happy, healthy and devoid of any complications at all. For most women who take proper prenatal care, get sufficient nutrition through a pregnancy diet, and follow a proper pregnancy exercise routine, this wish comes true. However, some women face complications such as miscarriage, stillbirth, obstetric cholestasis, pre-eclampsia and eclampsia, varicose veins, gestational diabetes, depression during pregnancy and infections.
Cervical insufficiency is one such complication, and it increases the risks of preterm labour and birth. Premature babies face a number of disease risks throughout their life, and their development can be slower. So, as preterm labour and birth are issues that are best avoided, keeping a check on your cervix and its insufficiency or incompetence is very important.
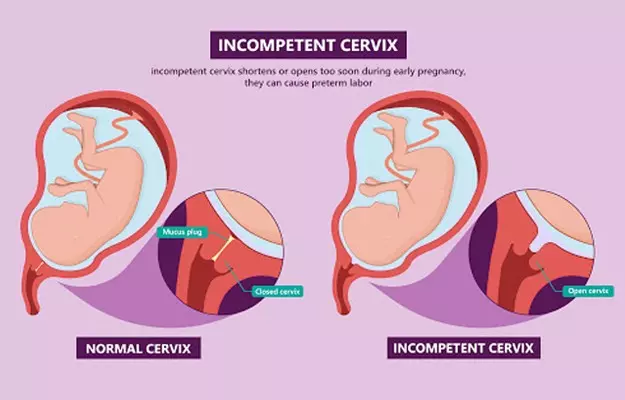
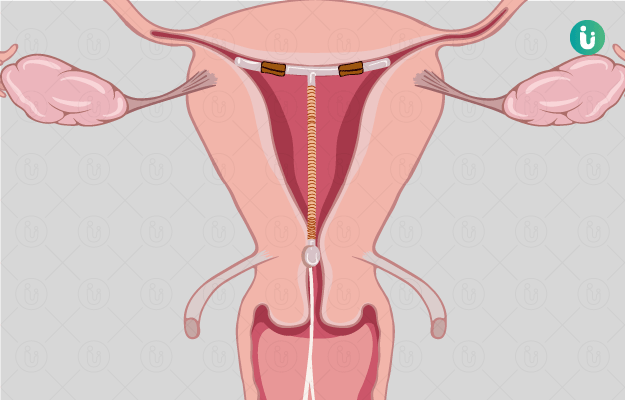
For those who don’t know, the cervix is the lower part of the uterus that connects to the vagina. This part naturally dilates or opens up when the body of a pregnant woman is ready for delivery. In normal circumstances, this dilation occurs a few days or weeks before the due delivery date. When you have cervical insufficiency, though, this dilation and simultaneous uterine contractions occur much earlier: even around the end of the second trimester or beginning of the third trimester.
Read more: Contractions during pregnancy
To be sure, cervical insufficiency is not something you can control. Genetic disorders that affect the production of collagen in the body have been linked to a weaker cervix. Women with uterine abnormalities may also experience insufficiency as the baby's weight grows to more than half a kilo or more towards the end of the second trimester. Cervical insufficiency is also quite common in women who are carrying twins or multiple foetuses.
An incompetent or insufficient cervix can be diagnosed as early as the 20th week of pregnancy—if you know what to look for and are aware of the risks involved with such a complication, or have a history of cervical insufficiency. On diagnosing cervical insufficiency, your obstetrician can recommend the most appropriate treatment for this complication, which is often cervical cerclage (not for women carrying twins, though). This is a small outpatient procedure with local anaesthesia, to sew the cervix shut for the remainder of the gestational period.
This small but significant procedure not only reduces the risk of preterm labour and birth, but it also ensures that the rest of your pregnancy is safe. Here’s everything you need to know about cervical insufficiency and cervical cerclage.