Summary
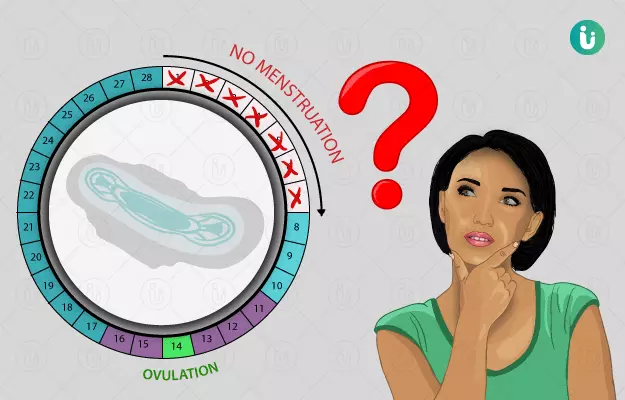
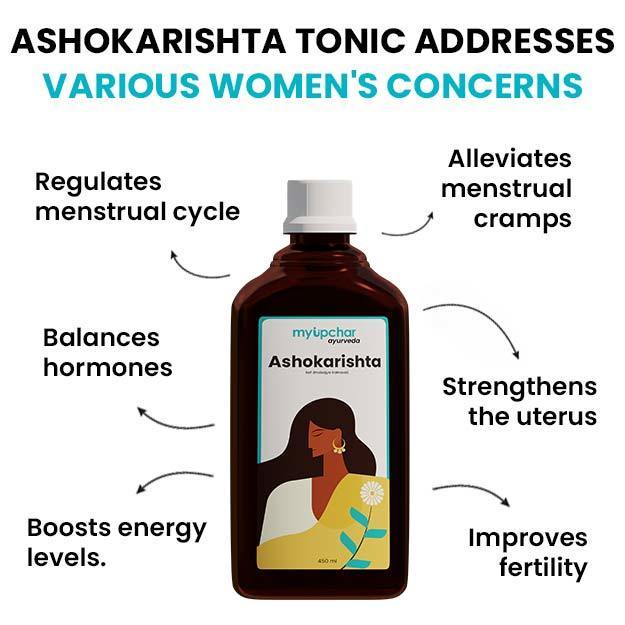
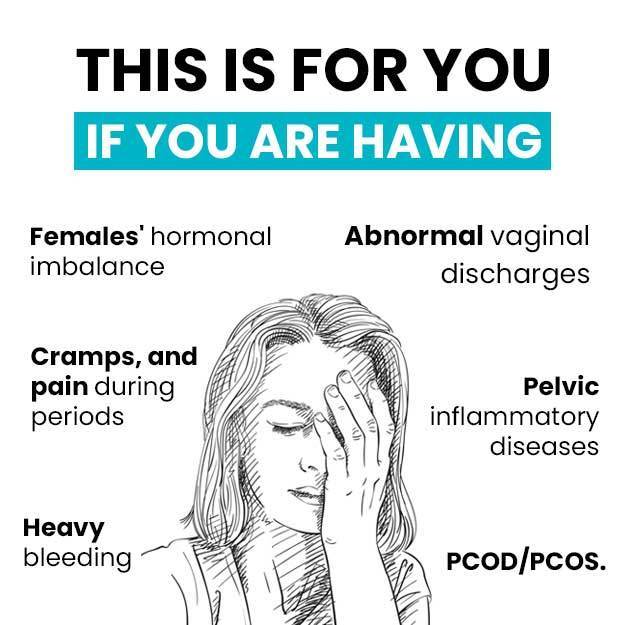
The menstrual cycle is a series of events, which occur each month during the reproductive age of a woman. It starts from puberty (12-14 years of age) and ends by around 45-50 years of age. If for any reason, menses don’t start at the time of puberty or stop completely before the termination age (menopause), the condition is termed amenorrhoea. Amenorrhoea can occur due to genetic or acquired causes like scar formation, the absence of a uterus or vagina, metabolic disorders, hormonal imbalance and more. Prevention might be possible for acquired conditions like Cushing’s syndrome and diabetes. Diagnosis consists of a physical examination, lab tests for hormone levels, endoscopy of the uterus, ultrasound and other imaging tests. Treatment consists of curing the underlying condition and might be difficult in the case of genetic disorders. Hormone replacement therapy is the mainstay of treatment in most cases. The outcome is good in most cases where the cause is not genetic.
(Read more: Light periods causes)