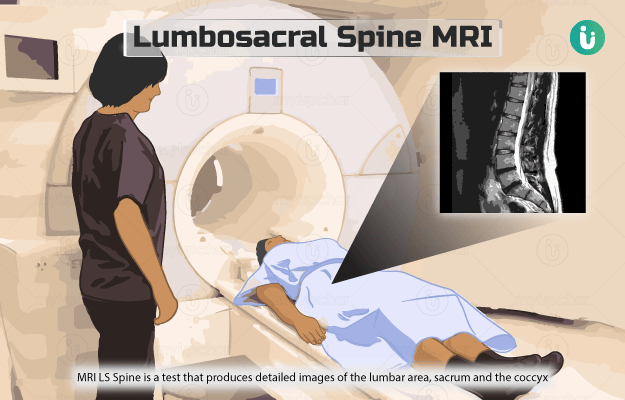
What is ankle joint magnetic resonance imaging (MRI)?
MRI of the ankle joint is a diagnostic test that uses a strong magnetic field, radio waves and a computer to produce clear images of the ankle joint.
The ankle joint connects the bones of our leg to the bones of our foot and allows us to move our foot up and down. It is reinforced by different soft tissues, such as:
- Ligaments: Strong tissues that hold the bones together.
- Tendons: Tissues that attach muscles to the bones.
- Cartilage: Smooth tissue that covers the ends of the bones.
- Synovium: A thin layer that lines the space within the joint.
Ankle joint MRI helps to detect injuries and abnormalities in the soft tissues and bones of the ankle. It is the preferred method to obtain good soft tissue images.
Your doctor may or may not use a contrast dye to perform this test. A contrast dye helps see images in better clarity (due to the contrast created) and is usually done in cases such as fractures, or cartilage or muscle tear.