What is Amenorrhoea Profile?
Amenorrhoea profile is a set of blood tests that are performed to determine the cause for amenorrhoea or the absence of monthly periods.
The monthly cycle in women starts at puberty (12-14 years of age) and only stops after the age of 50-55 (menopause). Pregnant women also don’t get periods. However, amenorrhea in any other phase of life may be a symptom of an underlying medical condition.
Amenorrhoea may be due to changes in the hormones, glands and organs that play a role in menstruation. It is of two types – primary amenorrhoea and secondary amenorrhoea.
Primary amenorrhoea is when a woman does not get her period by the age of 16. It may be due to:
- Underdeveloped reproductive organs
- Problems with the secretion of hormones by the pituitary gland and hypothalamus (parts of the brain that produce hormones involved in menstruation)
- Failure of the ovaries (female sex organs)
In many cases, the cause for primary amenorrhoea may not be known.
In secondary amenorrhoea, a woman with normal menses stops getting her monthly period due to any of the following causes:
- Breastfeeding
- Pregnancy
- Menopause
- Certain medicines and birth control methods
- Stopping the use of birth control pills
- Depression
- Stress
- Malnutrition
- Extreme weight loss or weight gain
- Ongoing illness
- Over-exercising
- Tumours in the ovaries
- Problems in the glands that produce hormones, including the thyroid
- Previous uterine surgery with scarring
A woman will also stop getting periods if she has had her ovaries or uterus removed.
If you are tired of dieting and exercising and are not able to lose weight, then use myUpchar Ayurveda Medarodh Fat Burner Capsule, it has no side effects, order it today and avail the benefits.
For the amenorrhoea profile, the blood levels of the following hormones are tested:
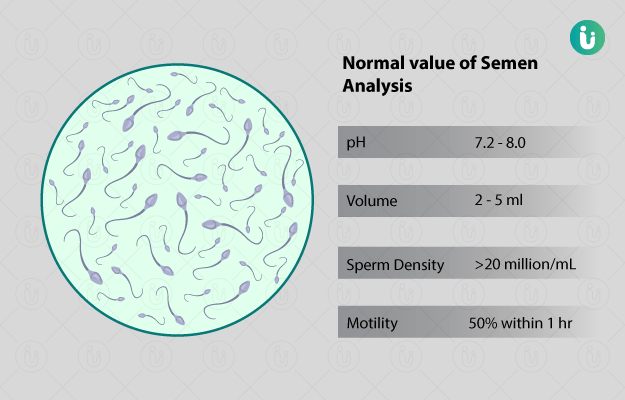
- LH: LH is an important reproductive hormone secreted by the pituitary gland, a small gland situated in your brain. It helps maintain the function of ovaries and triggers ovulation.
- FSH: Just like LH, FSH is also secreted by your pituitary gland. It stimulates the growth of eggs in the ovaries and helps in controlling the menstrual cycle. The levels of FSH vary during the menstrual cycle. If the levels are too low or too high, it could lead to menstrual difficulties. FSH also helps in the development of ovaries organs during puberty.
- Prolactin: Prolactin is yet another hormone that is released by your pituitary gland. It causes the breasts to develop and produce milk for the new-born. In women who are not pregnant, prolactin helps in regulating the menstrual cycle. High prolactin levels may cause amenorrhoea.
- TSH: The pituitary gland produces TSH, which stimulates the thyroid gland to produce two hormones (T3 and T4) that regulate several body functions. Thyroid is a butterfly-shaped gland present in our neck. If your TSH levels are too high or too low, it can affect your menstrual cycle.
A pregnancy test is also performed with the amenorrhoea profile to rule out pregnancy as a possible cause of the condition.