Summary
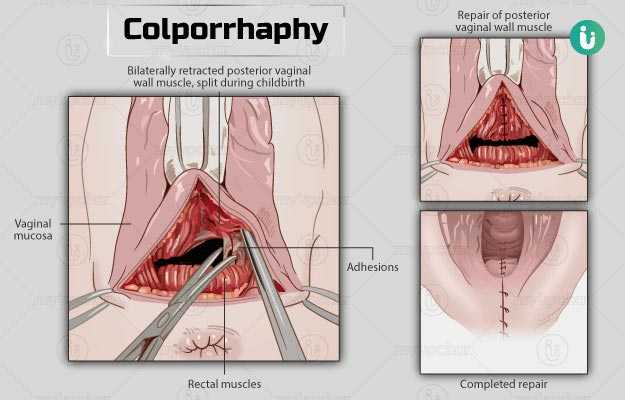
Colporrhaphy is a surgery recommended in women with pelvic organ prolapse. In this condition, the supporting tissues that hold the pelvic organs (uterus, urinary bladder, etc.) in their original position become weak. This leads to the bulging of the pelvic organs into the wall of the vagina, which causes pain or discomfort in the vagina, difficulty in controlling urine, and affects sexual life. Colporrhaphy involves repairing the supporting tissues between the vagina and pelvic organs with strong stitches. It helps to hold the pelvic organs back in their original position and provides relief from the symptoms of pelvic organ prolapse. The operation lasts for around 90 minutes, and you will be hospitalised for about one to two days after the surgery. You will have a follow-up appointment after two to three weeks of surgery to review your condition.