Pregnancy is a time of joy and great expectations for all women. Every mother-to-be is told to be extra cautious during the nine months of pregnancy, and this includes following a proper diet, exercise routine, check ups during pregnancy, etc. Getting ample rest and sleep during this period is equally necessary to make sure that there are no complications.
However, no matter how much care you might take, some complications can appear unless you actually live in a bubble. These complications can occur due to genetic factors, personal history or due to the immense changes in the body that are natural in pregnancy. Obstetric cholestasis, also known as intrahepatic cholestasis of pregnancy (ICP), is one such health complication that can arise during pregnancy.
Read more: Cholestatic Liver Diseases
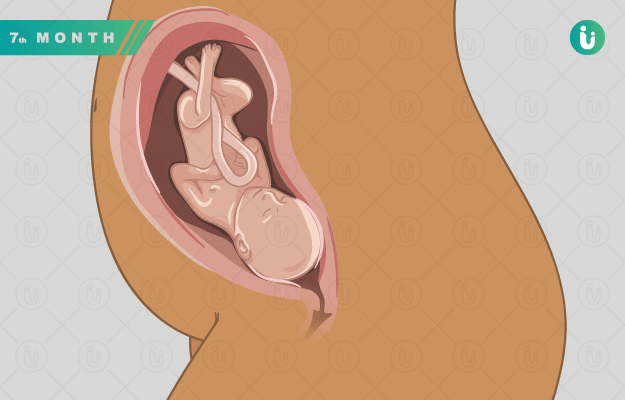
According to the American Pregnancy Association (APA), ICP is a liver disease in which the normal flow of bile is disrupted. During pregnancy, this disruption is likely to happen due to the increased amounts of pregnancy hormones, including estrogen and progesterone. Cholestasis usually occurs during the third trimester, but it can occur in the second trimester of pregnancy as well.
Studies suggest that women from the Indian subcontinent are at a higher risk of developing obstetric cholestasis, which means all Indian pregnant women should be aware of this complication of pregnancy and take precautions against it. This is important because obstetric cholestasis can cause foetal distress, premature birth and even stillbirth. Here is everything you need to know about this complication of pregnancy.
- Causes of cholestasis in pregnancy
- Symptoms of cholestasis in pregnancy
- Can obstetric cholestasis harm my baby?
- Diagnosis of cholestasis in pregnancy
- Treatment of cholestasis in pregnancy
- Can you get cholestasis during your next pregnancy?
Causes of cholestasis in pregnancy
According to the Royal College of Obstetricians and Gynaecologists and Obstetricians (RCOG), the exact causes behind obstetric cholestasis are not known. Doctors, however, suspect that there are two underlying causes behind the occurrence of obstetric cholestasis in pregnancy.
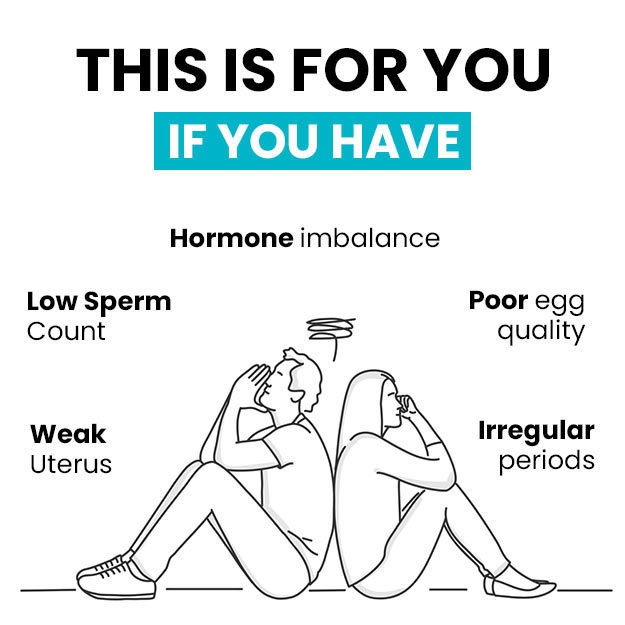
- Hormonal factors: According to the APA, hormonal imbalance - especially due to high levels of estrogen and progesterone - can affect liver function. A spike in these hormones can slow down or completely stop the flow of bile, which plays the vital function of breaking down fats during digestion. Due to hormonal changes in pregnancy, the bile flow is affected and this leads to the buildup of bile acids in the liver, from where it can then leak into the bloodstream.
- Genetic factors: The RCOG reveals that women from certain ethnic groups, especially women from the Indian subcontinent, are at an increased risk of developing cholestasis during pregnancy. If this complication runs in the family, it can again increase your chances of contracting it as well. It’s also likely that if you have suffered from cholestasis during a pregnancy, the disease might occur in your other pregnancies as well.
Can obstetric cholestasis harm my baby?
Obstetric cholestasis can cause foetal distress, which in turn can harm the baby in the three ways mentioned below.
- Increased chances of your baby passing meconium while in the womb. While babies usually pass urine into the amniotic fluid, ingest it and release it again, meconium refers to bowel movements as well. This can change the colour of the amniotic fluid into green or brown colour.
- According to the RCOG, one in 10 women with obstetric cholestasis may deliver their baby prematurely, i.e. before 37 weeks of gestation are completed. Premature labour and birth can have long-term effects on the health of the baby, including slow development, low birthweight, etc.
- The RCOG reveals that some studies indicate that obstetric cholestasis can cause stillbirth if labour is induced too early, i.e. before 23 weeks of pregnancy are complete. Proper prenatal care and neonatal care of the premature baby can reduce the risk of this effect.
Diagnosis of cholestasis in pregnancy
Most pregnant women usually show up with unexplained itching in the hands and feet, and this leads to their diagnosis. Once dermatological causes are ruled out, an obstetrician will recommend liver function tests (LFT) and bile acid and bilirubin level tests. If these levels are considered to be too high, especially in the absence of a pre-pregnancy liver disease, then obstetric cholestasis is confirmed and treatments recommended.
It’s possible that some women might have itching symptoms before their LFT show abnormal results. If no dermatological cause is found and the itching persists, then LFTs must be repeated every one or two weeks until the cause is diagnosed properly.
Treatment of cholestasis in pregnancy
Obstetric cholestasis has one treatment: the safe delivery of your baby, which will bring the hormonal levels back to normal and naturally cure the condition. However, managing the symptoms of obstetric cholestasis during the remainder of the gestation period is important. Most of these treatment options do not pose any effects The following treatment options might be given to you to manage the symptoms of cholestasis in pregnancy.
- Topically applicable anti-itching lotions or gels prescribed by the doctor
- Medications to decrease the concentration of bile acids in the body
- Vitamin K supplements to prevent intracranial hemorrhage or blood clotting issues
- Antihistamines to help sleep better and control itching
- Cool baths and loose-fitting clothes to reduce itching
- Non-stress tests, including fetal heart monitoring, to make sure the baby is fine
- Regular blood tests to monitor liver function, bile acids, etc.
Can you get cholestasis during your next pregnancy?
While there is no guarantee, it’s highly likely that you will get obstetric cholestasis in a future pregnancy if you have experienced it in a previous or current one. The RCOG recommends that women with a history of obstetric cholestasis should avoid taking contraceptive pills which have high estrogen levels in between two pregnancies. Instead, discussing alternative contraception methods is advisable to reduce the risk of obstetric cholestasis.
Find Gastroenterologist in cities
- Obstetrician and Gynaecologist in Bangalore
- Obstetrician and Gynaecologist in Mumbai
- Obstetrician and Gynaecologist in Ghaziabad
- Obstetrician and Gynaecologist in Chennai
- Obstetrician and Gynaecologist in Pune
- Obstetrician and Gynaecologist in Delhi
- Obstetrician and Gynaecologist in Hyderabad
- Obstetrician and Gynaecologist in New Delhi
- Obstetrician and Gynaecologist in Gwalior
- Obstetrician and Gynaecologist in Gurgaon
Doctors for Obstetric cholestasis

Dr. Ayushi Gandhi
Obstetrics & Gynaecology
4 Years of Experience

Dr. Anjali
Obstetrics & Gynaecology
23 Years of Experience

Dr.Anuja Ojha
Obstetrics & Gynaecology
20 Years of Experience

Dr. Geeta Kulkarni
Obstetrics & Gynaecology
7 Years of Experience
References
- Royal College of Obstetricians and Gynaecologists [Internet]. London, United Kingdom; Obstetric cholestasis
- National Health Service [Internet]. UK; Itching and intrahepatic cholestasis of pregnancy
- Milkiewicz, Piotr. et al. Obstetric cholestasis. BMJ. 2002 Jan 19; 324(7330): 123–124. PMID: 11799014
- Oxford University Hospitals. National Health Service [Internet]. UK; Obstetric Cholestasis (Itching Liver Disorder)
- American Pregnancy Association [Internet]. Irving, Texas, USA; Cholestasis Of Pregnancy
- Dang, Arbinder. et al. Prevalence of liver disease in pregnancy and its outcome with emphasis on obstetric cholestasis: An Indian scenario. J Obstet Gynaecol India. 2010 Oct; 60(5): 413–418. PMCID: PMC3394613