Molar pregnancy or hydatidiform mole is a condition in which a part or whole of the placenta starts to grow unusually. It is a type of gestational trophoblastic disease.
Trophoblasts are the cells that the placenta is made of. Gestational, as you know, is anything pregnancy-related. Trophoblastic disease refers to a group of conditions wherein tumours develop in the womb from the placenta.
Molar pregnancy is an uncommon condition—it affects about 1 in every 800-1,000 pregnancies—and it usually occurs due to a genetic error in the fertilization process. In some cases, there is no development of foetal tissue. In others, miscarriage occurs early in the pregnancy. (Read more: Chemical pregnancy symptoms, causes, treatment)
A woman with a molar pregnancy usually has all the signs of pregnancy. That is why a lot of women do not get to know about them until after a miscarriage. Most women with a molar pregnancy miscarry by the end of the first trimester. However, for some, the mole may also show up on an ultrasound.
Hydatidiform moles are generally not harmful but if left untreated, the affected tissue can spread to other parts of the body (through the blood) including the lungs, brain and liver. In rare cases, it can turn cancerous.
The condition is usually treated through medications and surgery.
- What is a molar pregnancy?
- Types of molar pregnancy
- Causes and risk factors of molar pregnancy
- Symptoms and signs of molar pregnancy
- Diagnosis of molar pregnancy
- Treatment of molar pregnancy
- Complications of a molar pregnancy
What is a molar pregnancy?
During fertilisation, the sperm fuses with the egg inside the fallopian tube and forms an embryo. The sperm and ova each carry half the genetic information for the foetus. Each cell in the human body has 23 pairs of chromosomes, so every sperm and ova have at least 23 chromosomes. Out of these, one pair is that of sex chromosomes. Females have two X chromosomes (XX) as their sex chromosomes while males have an X and a Y chromosome (XY).
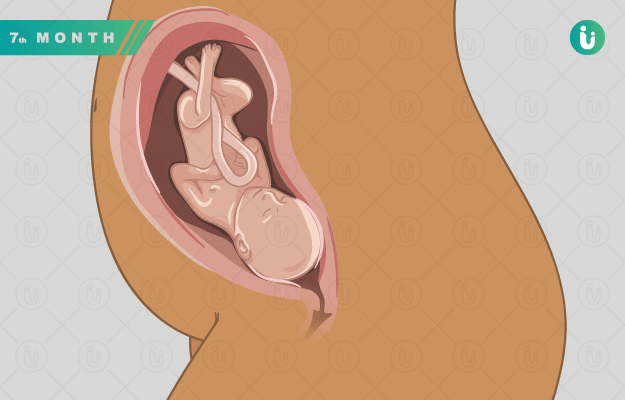
The outer layer of this embryo forms the placenta—the structure through which the foetus breathes, eats and exchanges oxygen and carbon dioxide. The inner part of the embryo forms the foetus.
However, in the case of molar pregnancy, the embryo gets an abnormal number of chromosomes. This shows up as unusual growth of placenta with or without the foetus. The placenta may become larger than normal and may also have fluid-filled sacs called cysts.
Types of molar pregnancy
Depending on how much of the embryo starts to have abnormal growth, molar pregnancy is of two types:
- Complete molar pregnancy: A complete molar pregnancy happens when a sperm fertilises an empty egg. Since the fertilisation never actually took place, no foetus is formed in this case. Instead, the supposedly fertilised mass is just placental tissue.
The single sperm duplicates itself and the mass so formed still has 23 pairs of chromosomes, usually with XX sex chromosomes. Sometimes two sperms fuse with the ova. - Partial molar pregnancy: In a partial molar pregnancy, the foetus or foetal tissue is also a part of the abnormal mass. These moles form when two sperms fuse with an ovum. The total number of chromosomes in such an embryo is 69, including three sex chromosomes which could be XYY, XXX or XXY.
In cases of twins, sometimes only one embryo is the mole while the other one is normal. However, the latter is soon taken over by the abnormal cells.
Read more: Twin pregnancy
Causes and risk factors of molar pregnancy
The exact cause of molar pregnancy is unknown. However, according to The Royal Women’s Hospital, Australia, the following are some of the risk factors for molar pregnancy:
- Nutritional deficiency
- Being older than 40 years or younger than 20 years of age at the time of conceiving
- Asian background
- A history of molar pregnancy
Symptoms and signs of molar pregnancy
A woman with molar pregnancy usually does not even realise till 12-16 weeks that there is something wrong with the pregnancy. Since the placenta is releasing HCG, she would have all the initial symptoms of pregnancy.
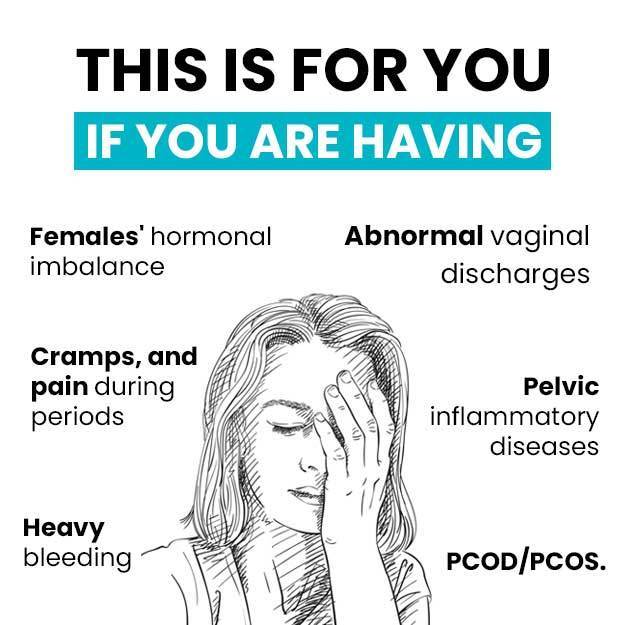
However, some early signs of a molar pregnancy include:
- Excess or dark vaginal discharge during pregnancy
- Vaginal bleeding that could be dark brown to bright red in colour
- Abnormal appearance of the uterus in the first pregnancy ultrasound
- Severe morning sickness
Some later symptoms of a molar pregnancy include:
- Lack of fetal movement and heartbeat
- Larger than normal size of uterus as per the pregnancy month
- High blood pressure (hypertension)
- Hyperthyroidism or excess thyroid hormone in the body
Diagnosis of molar pregnancy
In most cases, a woman would get a miscarriage and would only know about the molar pregnancy when the placental tissue is tested under a microscope.
The condition may also be diagnosed by:
- Physical examination: The uterus may feel too big for the month of the pregnancy. It could also feel softer. On examination with a speculum, the doctor may notice cervical dilation or presence of grape-like particles.
- Basic metabolic panel: The doctor may advise a basic metabolic panel (a blood test) to check kidney function and electrolyte abnormalities.
- Blood and urine test: Higher than normal hCG levels show up in these tests in case of a molar pregnancy. Human chorionic gonadotropin or hCG is a hormone that the embryo produces to form the placenta—pregnancy home kits check for the presence of this hormone in urine. (Read more: Beta hCG test)
- Thyroid tests: Your doctor may ask you to get a thyroid function test, to check for hyperthyroidism.
- Liver test: A liver function test may be advised to check for proteinuria (presence of protein in urine) in case the doctor suspects preeclampsia.
- Pelvic ultrasound: A partial mole may show a foetus but the placenta would be enlarged and will have cysts with a swiss cheese-like appearance.
The doctor may also ask you about your medical history. If the doctor suspects that the mole has turned invasive and has spread to nearby areas, he/she may also suggest other tests including a CT scan and an MRI scan.
Treatment of molar pregnancy
In most cases, a molar pregnancy spontaneously terminates (miscarriage) by the fourth month. In such cases, a doctor would suggest a minor procedure called dilation and curettage (D&C) to remove any remaining tissue in your body. In this procedure, your doctor will give you general or regional anaesthesia and insert a sharp instrument called a curette into your cervix to scrape your uterus lining.
In case the miscarriage does not happen and a molar pregnancy is identified, your doctor will give you medications so that your uterus releases the pregnancy. D&C will be done once that happens.
A third treatment called vacuum aspiration is used if the medications don’t work either. Vacuum aspiration is just like D&C. However, in this procedure, a hollow tube called a cannula is passed into the uterus through the cervix. The cannula is attached to a pump and a bottle that apply suction. Through this suction and the use of a small instrument called a curette, the molar tissue is slowly removed. The procedure is done under general anaesthesia, so you will be asleep the whole time and your doctor will give you medications to bring your uterus size to normal after the procedure and to stop the bleeding.
Finally, women who do not want a baby in the future are suggested a hysterectomy.
Follow up
Even after the treatment, your doctor will check your hCG levels for up to six months. Most women are advised against conceiving for this duration.
Higher hCG levels even after the pregnancy can indicate that traces of moles are still present in the body. It is important to remove all the traces of the mole to keep it from turning cancerous.
Complications of a molar pregnancy
Hydatidiform moles are usually non-invasive or benign. However, 1-2% cases of partial molar pregnancy and 15-20% cases of complete molar pregnancy turn invasive.
Persistent gestational trophoblastic disease is when a part of the mole remains in the body even after treatment and grows into the muscle layer beneath the uterine lining.
In rare cases, the condition worsens to choriocarcinoma where the abnormal tissue turns cancerous. The cancer cells can spread to any part of the body. Hence it is important to identify and clear out all the remains of the mole.
The condition may recur in some women.
Find Obstetrician and Gynaecologist in cities
- Obstetrician and Gynaecologist in Bangalore
- Obstetrician and Gynaecologist in Mumbai
- Obstetrician and Gynaecologist in Ghaziabad
- Obstetrician and Gynaecologist in Chennai
- Obstetrician and Gynaecologist in Pune
- Obstetrician and Gynaecologist in Delhi
- Obstetrician and Gynaecologist in Hyderabad
- Obstetrician and Gynaecologist in New Delhi
- Obstetrician and Gynaecologist in Gwalior
- Obstetrician and Gynaecologist in Gurgaon
References
- American Cancer Society [internet]. Atlanta (GA). USA; What Is Gestational Trophoblastic Disease?
- the Women's: The Royal Women's Hospital. Victoria. Australia; Hydatiform mole
- Better health channel. Department of Health and Human Services [internet]. State government of Victoria; Molar pregnancy
- Heleen van Beekhuizen. Molar Pregnancy and other Gestational Trophoblastic Diseases. The Global Library of Women's Medicine [Internet].
- MedlinePlus Medical Encyclopedia [Internet]. US National Library of Medicine. Bethesda. Maryland. USA; Choriocarcinoma
- Ghassemzadeh S, Kang M. Hydatidiform Mole. [Updated 2019 Jun 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Johns Hopkins Medicine [Internet]. The Johns Hopkins University, The Johns Hopkins Hospital, and Johns Hopkins Health System; Dilation and Curettage (D and C)
- CardioSmart: American College of Cardiology [Internet]. Washinton D.C. US; Vacuum Aspiration for Molar Pregnancy
- American Pregnancy Association [internet]; Molar Pregnancy
- Ministry of Health: Government of New Zealand [Internet]. New Zealand; Molar Pregnancy: Patient information booklet