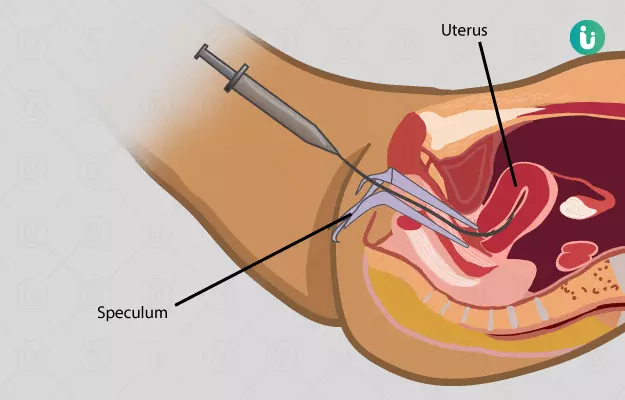
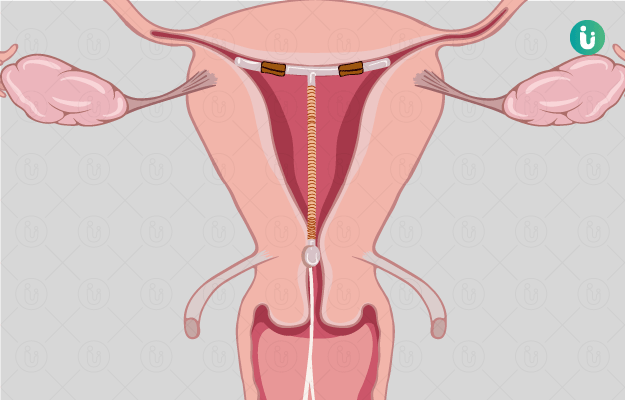
Intrauterine insemination (IUI) is a method of assisted reproductive technology (ART) used to treat infertility. The procedure results in in-vivo fertilisation of the egg with the sperm.
It is a feasible method of ART compared to other methods which are pretty expensive though it may require multiple cycles of treatment.
The procedure is of short duration and hence is conducted as a daycare admission. Follow-up is often stressful since the patient is anxious to know whether the procedure was successful. Hence, counselling is an important aspect of the process.