What is Wilson’s disease?
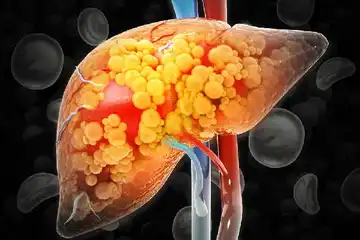
Wilson’s disease is a rare, inherited metabolic disorder involving dysfunction in copper metabolism that leads to copper accumulation in vital organs such as the brain and the liver. The disorder occurs more commonly in males and is seen during adolescence. The disease was first described by British neurologist Dr Samuel Alexander Kinnier Wilson, hence, the name.
What are its main associated signs and symptoms?
The main signs and symptoms of Wilson’s disease include:
- Impaired neurocognitive functions
- Jaundice
- Abdominal pain and swelling
- Nausea
- Vomiting blood
- Depression
- Anxiety
- Mood swings
- Difficulty in speaking
- Tremors
- Body stiffness
- Problems with balancing
- Rusty brown rings around the iris, Kayser-Fleischer
- Portal hypertension- high blood pressure in the portal venous system that connects the liver and the spleen
- Cirrhosis
- Spider naevi (small distended blood vessels, usually on the chest and the abdomen)
- Severe acute liver failure
- Ammonia in the bloodstream
- Hepatic encephalopathy (confusion, coma, seizures and finally life-threatening swelling of the brain due to liver disease)
- Seizures
What are the main causes?
Wilson’s disease is caused due to mutations in Wilson’s disease protein (ATP7B). An abnormal copy of genes with mutation is present in at least one parental gene, who are carriers. Only if both the parents inherit this recessive gene, the child will have Wilson’s disease.
Copper is required by the body, as it is an important cofactor for various metabolic processes. The copper binding protein (ATP7B) is essential for binding of copper in the liver and removal of excess copper through bile. However, in patients with Wilson’s disease, there is impairment of the Wilson’s disease protein due to genetic mutations, which causes accumulation of copper and oxidative damage of the liver cells and tissues. Precipitation of copper is also seen in the brain, thereby affecting neurocognitive functions.
How is it diagnosed and treated?
The diagnosis of Wilson’s disease includes:
- Biochemical tests: Liver function tests, estimation of serum copper, serum ceruloplasmin and 24-hr urinary copper, renal function tests, and haematological (blood) investigations.
- Ophthalmological evaluation: Slit lamp evaluation for Kayser-Fleischer (KF) ring.
- Neurophysiological evaluation.
- X-ray: To evaluate skeletal abnormalities
- Computed tomography (CT scan of brain)
- Magnetic resonance imaging (MRI) of brain
- Genetic testing
Treatment of Wilson’s disease aims to prevent excess accumulation of copper, either by decreasing its intestinal absorption or increasing its urinary excretion. Treatment with D penicillamine, mobilizes copper and forms copper–penicillamine complexes that are excreted in the urine. Using a copper chelator helps to bind excess copper. Zinc increases levels of intestinal cell metallothionein, a protein with strong affinity for binding copper in the intestine and decreasing its intestinal absorption. Tetrathiomolybdate complexes copper in the intestinal lumen preventing its absorption. It complexes copper with albumin in the blood and makes the copper unavailable for cellular uptake. The ultimate treatment option for patients with Wilson’s disease is liver transplantation.

 OTC Medicines for Wilson's Disease
OTC Medicines for Wilson's Disease