Summary
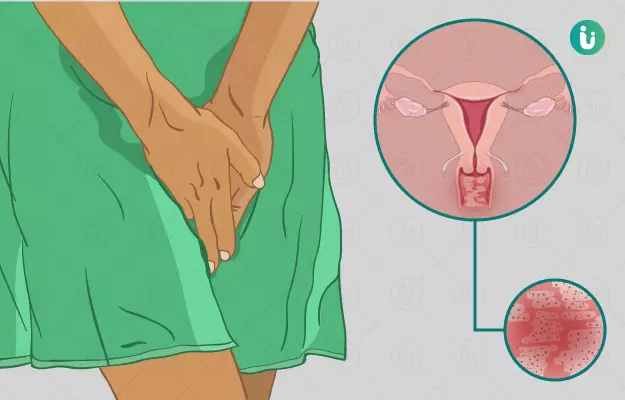
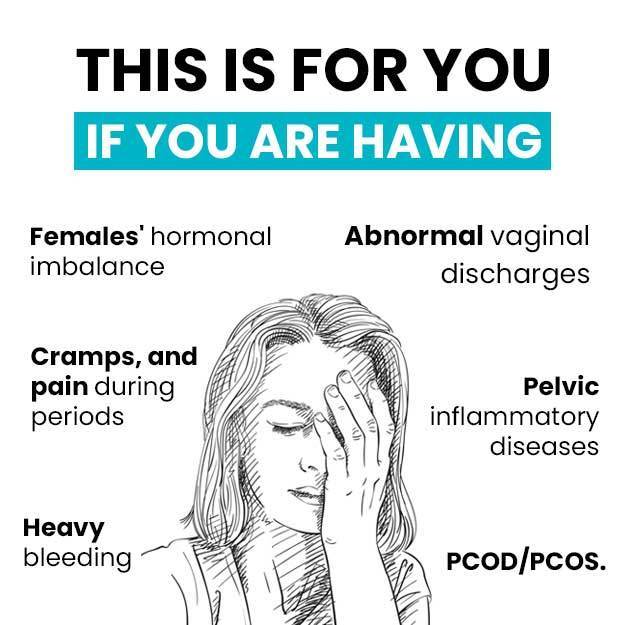
Vaginitis is an inflammation or swelling of the vagina and the adjoining vulva in women of reproductive age. It is generally caused by a bacterial or fungal or parasitic infection. Sometimes, it may occur due to an allergic reaction to products like creams or inserted contraceptive devices. In vaginitis, there is swelling, irritation, redness, and itching in the vagina and vulva along with abnormal vaginal discharge. Diagnosis is made by observing the signs and symptoms. If required, a microscopic examination of the vaginal swab can be performed to find out the exact cause of vaginitis. The condition is treated by local application of antibiotics and in chronic cases, oral antibiotics can be used. The outcome is generally good as it is completely treatable.
Complications of vaginitis include recurrence of infection following treatment, superinfection by other pathogens (harmful microorganisms), and rarely, the spread of infection to the uterus. Maintaining adequate vaginal hygiene is important to prevent vaginitis.
(Read more: Tips on keeping your vagina healthy)