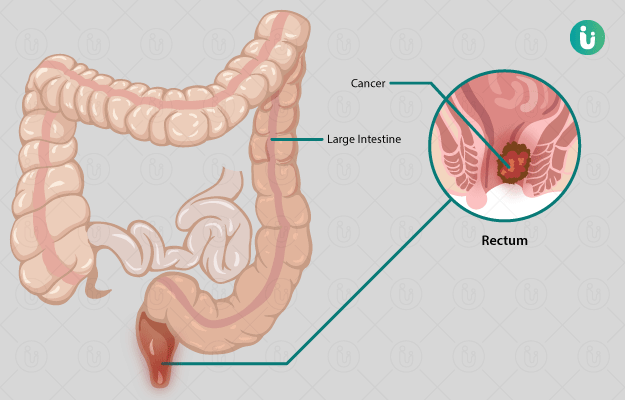
Cancer that starts in the rectum or the final portion of the large intestine is called rectal cancer. It is part of a larger group of cancers called colorectal cancer, which involves the colon and the rectum. The gut, or the digestive tract, begins at the mouth, through which food is passed into the esophagus. Through the esophagus, the food enters the stomach, where some of it is digested. The contents of the partially digested food are then passed into the small intestine for further digestion. After all the food is digested, it is passed to the large intestine or the colon. Here, water and other substances are absorbed and the final waste product is removed from the bowel through the rectum and out of the body from the anus.
New Year Bumper Sale @ Rs. 1
X

- हिं - हिंदी
- En - English
- Treatment
-
- Skin Issues
- Acne
- Fungal Infection
-
- Hair Problems
- Hair Growth
- Hair Dandruff
- Self-Analysis
-
- Chronic Diseases
- Diabetes
- Heart Care
- Weight Loss
- Sleep Support
- Liver Care
- Stress & Anxiety
- Our Brands
- Doctor Consultation
- Medicine A-Z
-
Health A-Z
-
- Treatments
- Home Remedies
- Herbs
- Surgery
- Lab Test
- Therapy
- First Aid
- Ayurveda
- Homeopathy
-
- Yoga And Fitness
- Fitness
- Yoga
- Weight Loss
- Weight Gain
-
- Other Topics
- Baby Names
- Beauty
- Healthy Foods
- Tips
- Health News
- Pet Health
- Men Health
- Medical Cannabis
- Login / Sign Up
 Doctors for Rectal Cancer
Doctors for Rectal Cancer  OTC Medicines for Rectal Cancer
OTC Medicines for Rectal Cancer