Summary
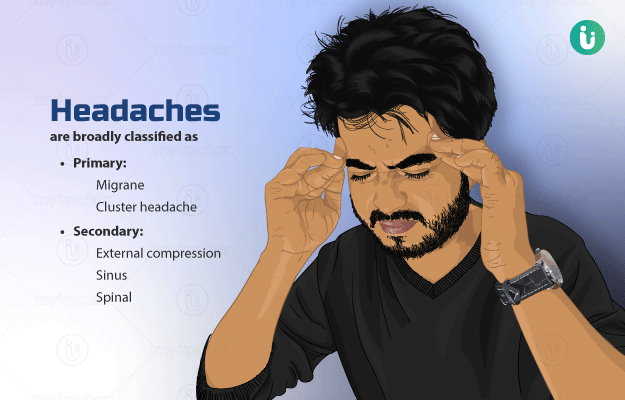
Headache is the symptom of pain involving any area of the head or neck. It may involve one or both sides of the head, be pinpointed to a particular area or spread from a single point, Most of the headaches appear as sharp or dull, lasting for minutes or even days. The evaluation of a headache can be straightforward or challenging. Although most of the times headaches are harmless, they can sometimes be a manifestation of a severe underlying illness. Headaches can be of primary or secondary. Primary headaches do not have a known cause; whereas headaches are associated with underlying pathologies or conditions, which cause traction or inflammation of the underlying structures. Different types of headaches usually present with a specific set of symptoms, occur uniquely, and therefore require tailor-made treatments.

 Doctors for Headache
Doctors for Headache  OTC Medicines for Headache
OTC Medicines for Headache
 Headache articles
Headache articles
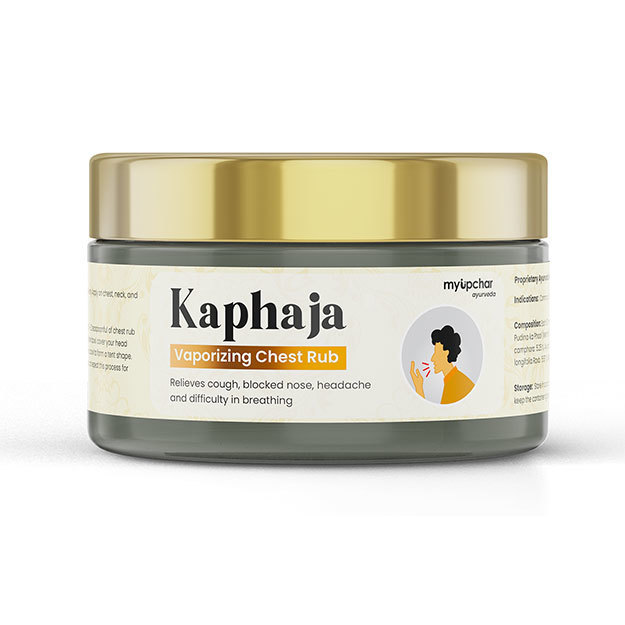
 Ayurvedic Treatment of Headache
Ayurvedic Treatment of Headache
 First Aid for Headache
First Aid for Headache
 Home Remedies for Headache
Home Remedies for Headache
 Homeopathic Treatment of Headache
Homeopathic Treatment of Headache




















 Editorial Team
Editorial Team