Vaginal health is a reflection of the overall health of your body. But, a lot of women aren't quite comfortable talking about it. Some may even ignore common symptoms of infection, making the situation worse for them. Did you ever have a problem checking in with a doctor about a fever or a cold? Then you should not feel ashamed or awkward talking about your vaginal health as well. It is the 21st century, after all, humans boast of wireless technology and high tech health services, it’s high time that you stop overthinking on trivial matters and take our health a bit more seriously.
An unhealthy or sick vagina brings with itself a lot of troubles which includes but are not limited to reduced orgasm, vaginal pain, loss of sexual desire and may even pose a threat to your fertility. Thinking of the last time you ignored an itchy vagina?
There are a lot of misconceptions and lack of information when it comes to vaginal health. This article focuses on debunking some of those myths along with telling you the best possible ways to maintain a healthy vagina.
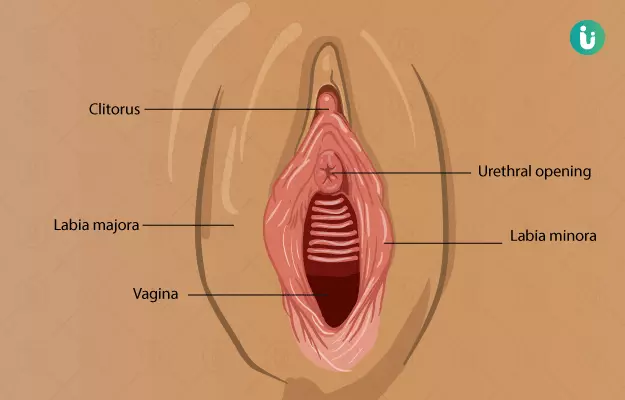
Know your vagina
Vagina is a muscular tube, about 3 inches in length, which runs from your cervix (a narrow tube that opens into the uterus) to the vaginal opening between legs. It is quite flexible and varies in shape and size in different women. Vagina shapes range from oval to cylindrical and it may be a light pink to almost a brownish red-pink in some. Also, the size of the vaginal labia (the lips that are present outside your vagina) may vary but all of it is quite normal as long as it doesn’t affect the normal functioning of your vagina.
Vagina and vulva are often interchangeably used to denote female genital organs however these do not refer to the same thing. While vulva refers to the entire external female genitalia, including pubis, labia and clitoris, the vagina is just a tube that runs to the uterus. It is the same tube that facilitates the secretion of menstrual fluid and through which the child comes out at the time of delivery.
Vaginal discharge
Vaginal discharge refers to the mucus secreted by the cervix and it is important to maintain the self-cleansing capacity of the vagina, which inhibits bacterial growth and infections. There are usually a lot of questions when it comes to vaginal discharge pertaining to what is normal and what is not. Here are some pointers that may help you understand it.
Vaginal discharge is a clear white fluid that does not have an offensive odour. It could be thick and sticky or thin, slippery and wet.
The amount of discharge varies depending on the phase of menstrual cycle you are in. Some days you might have almost no discharge and other days it might be considerable. This also varies from person to person. However, if you are concerned about the amount of vaginal discharge, it is best that you talk to a gynae to understand what is normal for you.
If you notice a yellow, green or red colour, an unpleasant or a fishy smell or a very thick and more than normal discharge, it could be a sign of infection.
Spotting and brown discharge right after your period could just be a sign that your uterus is cleaning itself, though, if you notice clots more often, it is best that you refer to a doctor.
Spotting during ovulation may or may not point to an underlying condition.
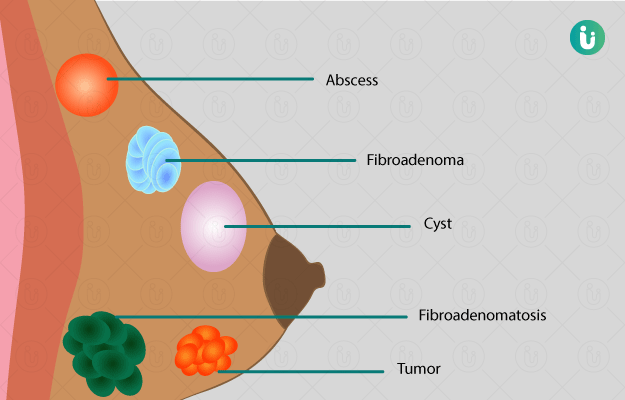
Vaginal diseases
Now you know what is normal when it comes to your vagina and its health. Let’s move on to vaginal diseases and when to contact a doctor.
Vaginitis
Vaginitis refers to the inflammation of the vagina. It is usually marked by swelling, itching and pain in the vagina and vulva. Though it could be caused by trichomoniasis, a sexually transmitted disease, the most common cause of vaginitis is the disruption of normal microflora.
Vaginitis is a common disease and a lot of women, especially in their reproductive age suffer from this problem.
So what causes this disruption in the normal bacterial population of the vagina?
Unprotected sex for once, may be responsible for this problem likewise having multiple sexual partners is. Some other factors that involved in vaginitis pathogenesis are:
- Antibiotics,
- Yeast infections or vaginal thrush,
- Bacterial infections or bacterial vaginosis,
- Intrauterine device,
- Hormonal imbalances,
- and douching
Furthermore, it may be caused by an allergy to a soap or detergent.
In some cases, more than one of these factors is involved in the pathogenesis of vaginitis.
Symptoms:
Vaginitis symptoms may not be as apparent when caused due to a bacterial infection. However, you may notice a fishy smell in the vaginal discharge. A yeast infection may manifest as a thick yellow vaginal discharge that looks like cottage cheese accompanied by redness and itching.
In case of trichomonas-induced vaginitis, you may or may not experience any apparent symptoms, but when it does, it is felt as itching and burning sensation while urinating, sore vagina and an unpleasant smelling greyish green vaginal discharge.
Vaginitis is usually treated by over-the-counter medications which include vaginal pills and creams. However, it is preferable that you refer to a doctor to understand the cause of vaginitis before popping any pill.
Sexually transmitted diseases affecting the vagina
Apart from the already mentioned problems, vagina may also be affected by some sexually transmitted diseases. As the name suggests, they spread from unprotected sex and multiple partners. Here is a list of some of the most common STDs along with their apparent symptoms.
Genital herpes
Genital herpes is mostly caused by the herpes simplex virus, HSV-2, which is also responsible for causing cold sores. Oral herpes is mainly caused by HSV-1, it can spread to the vagina through oral sex. In case of pregnancy, it is important to get them treated as early as possible since they have been known to cause miscarriage and mortality in newborns.
Symptoms:
Genital herpes appears in the form of tiny recurring sores around the genital area which may be associated with pain, though, most people do not notice any symptoms of herpes or they go unnoticed.
It is difficult to completely treat herpes symptoms especially if it’s caused by HSV-2, though, recurrent infections can be managed by medications.
Chlamydia
Chlamydia is yet another STD that is caused by the bacteria Chlamydia trachomatis. Commonly spread by oral, vaginal or anal sex, chlamydia poses a serious threat to the female reproductive system and may increase the chances of ectopic pregnancy and cause difficulty in conceiving. It may also cause infertility and pelvic inflammatory disease when left untreated.
Symptoms:
- Abdominal pain and post-sex bleeding
- Vaginal bleeding
- Painful urination
- Abnormal vaginal discharge
Chlamydia is completely curable with the right antibiotics, provided that you do not miss your medicine and take care of your vaginal hygiene. Also, it is best that you abstain from sex until your partner has been cleared of chlamydia.
Gonorrhoea
Gonorrhoea is a bacterial infection of vagina and vulva, which is usually symptom-free. It is spread by a vaginal, oral or anal sex. Some of the symptoms of gonorrhoea include vaginal bleeding, painful urination and increased vaginal discharge. Some people may also notice painful bowel movements and sore and itchy anus.
Gonorrhoea infection can be transferred to the foetus, so if you are pregnant, it is highly important to get adequate medical help.
Untreated gonorrhoea infections may lead to permanent damage to the reproductive system in the form of scars in fallopian tubes, infertility and ectopic pregnancies.
Gonorrhoea is usually treated by antibiotics. However, drug-resistant strains of this bacteria are quickly growing If you notice the persistence of symptoms for long, talk to your doctor to get the right treatment as soon as possible.
Genital warts
Genital warts is a common problem that is characterised by the formation of small papular growth around the vaginal wall. However, in some cases, they may be too small to be noticed. Usually caused by human papillomavirus (HPV) it may be associated with itching in the anal area and the genitals. It is spread by coming in contact with infected warts during sex.
Although HPV cannot be completely cured, genital warts are easily removed by surgical treatment which may be done by freezing, electric currents or lasers. It is a completely safe procedure when done by a trained medical practitioner.
Since the virus is still not cleared out of the system recurrences are common.
Vaginismus
Vaginismus refers to the involuntary spasms that happen in vaginal muscles in response to penetration of any kind. This may occur while inserting tampons and during gynaecological examination. Rape, molestation and fear of pregnancy could be the responsible factors. Other factors which cause vaginal spasms are:
- STDs
- Urinary tract infections or UTIs
- Fear of getting hurt
- Childbirth
- Chronic pain syndrome
Vaginismus treatment includes psychotherapy and exercises to make one comfortable with penetration. Pelvic floor exercises and relaxation techniques are also used.
(Read more: Pain during sex)
Vaginal prolapse
Vaginal prolapse refers to a condition where the uterus, intestines and bladders come down through the vagina, sometimes even protruding out.
Common symptoms of vaginal prolapse include:
- Feeling a bulge in the vagina
- Constant pain in the lower back
- Difficulty in passing stools or urine
- Difficulty in intercourse
Vaginal prolapse may be caused due to old age or it may be due to obesity. Long-term constipation, pregnancy and delivery and lifting heavy weights are also some of the causative factors of vaginal prolapse.
It is usually treated by vaginal pessary (a device that fit inside the vagina to support the uterus) and pelvic floor exercises however they are not helpful in the long term and surgery is the best way to get the uterus and bowel back to their position.
Vaginal cancer
Vaginal cancer is marked by an abnormal growth of the vaginal cells. Though vaginal cancer is quite uncommon, age is one of the primary risk factors. It is characterised by vaginal bleeding, lump in the vagina, constipation, pelvic pain and painful urination. However, all of these symptoms may be indicative of other problems as well. It is important that you talk to your doctor before reaching any conclusion.
Vaginal cancer is usually diagnosed by a colonoscopy or a biopsy.
Vaginal tests
pH test
Vagina has an inherently acidic pH. pH refers to the acidity or the alkalinity of a substance. Lower pH generally goes in the acidic range while a higher pH denotes a basic or alkaline environment. Any disruption in the vaginal pH may leave your vagina prone to infections which manifest as itching, burning or vaginal odour. For a pH test, vaginal discharge is taken from the walls of vagina and put on a pH paper. It is then matched with a pH chart to get results. Fortunately, this test can be done at home by buying pH kits and it is as reliable as the hospital test. However, an elevated pH does not confirm a disease. So, it is recommended to get yourself diagnosed by a doctor.
Bacterial and yeast cultures
Microbial culture tests are done to ascertain the presence of and to identify infectious pathogens. For this test, vaginal secretions are collected during pelvic examination.
Vaginal care tips
Now that you know about the various conditions and infections that may affect your vagina and are well acquainted with your vagina, it would definitely be easier to sidestep and prevent most of the above-mentioned conditions. Still, there are some other things that may help in maintaining and improving vaginal health. Let us have a look at them.
- Although your vagina knows how to cleanse itself, it is best that you gently wash the external of your genitals with unscented mild soaps. These do not disrupt the pH and are non-harmful. Do not use very hot water and clean vagina towards from the front to the anal region to avoid bacterial transfer from anus to vagina.
- Douching is sometimes used to clean vagina with the help of water and fluids like vinegar. Despite being a popular trend among people, it negatively affects the normal pH of the vagina and impacts normal vaginal microflora. So, it is best to avoid douching. For the same reason, vaginal deodorants and swipes must be avoided. Talk to your gynaecologist if you experience unpleasant vaginal odour.
- Wear cotton underwear and do not wash them with hard detergents. Try avoiding thongs and synthetic underwear that may cause irritation.
- Stay away from tight-fitting clothes.
- Follow safe sexual practices by using an unused condom or a femidom. It is also essential to know about the sexual history of your partner.
- Visit your gynaecologist regularly, especially if you are sexually active.
- In case of vaginal dryness, use water-based lubricants to avoid a painful sexual intercourse.
- Overuse of antibiotics has a detrimental effect on vaginal health, which must be avoided. However, this does not mean that you don’t take pills if so prescribed.
- Practice Kegel exercises. These help in strengthening your pelvic floor muscles which support your uterus and bladder. They are also believed to improve orgasms.
- Take healthy food and a balanced diet and stay away from smoking, alcohol and junk food.
References
- National Health Service [Internet]. UK; Is my vagina normal?.
- Planned Parenthood Federation of America. How much vaginal discharge is normal?. [Internet]
- National Health Service [Internet]. UK; Vaginal discharge.
- MedlinePlus Medical Encyclopedia: US National Library of Medicine; Vaginitis
- Center for Disease Control and Prevention [internet], Atlanta (GA): US Department of Health and Human Services; Genital Herpes - CDC Fact Sheet
- National Health Service [Internet]. UK; Chlamydia.
- Center for Disease Control and Prevention [internet], Atlanta (GA): US Department of Health and Human Services; Gonorrhea - CDC Fact Sheet
- Office on Women's Health [Internet] U.S. Department of Health and Human Services; Genital warts.
- Office on Women's Health [Internet] U.S. Department of Health and Human Services; Genital warts.
- healthdirect Australia. Vaginismus. Australian government: Department of Health
- National Health Service [Internet]. UK; Vaginismus.
- National Health Service [Internet]. UK; Having a pessary for a vaginal prolapse .
- National Cancer Institute [Internet]. Bethesda (MD): U.S. Department of Health and Human Services; Vaginal Cancer Treatment (PDQ®)–Patient Version Go to Health Profes
- U. S Food and Drug Association. [Internet]. Vaginal pH
- Kelly KG. Tests on Vaginal Discharge. In: Walker HK, Hall WD, Hurst JW, editors. Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition. Boston: Butterworths; 1990. Chapter 179.
- National Health Service [Internet]. UK; Keeping your vagina clean and healthy.