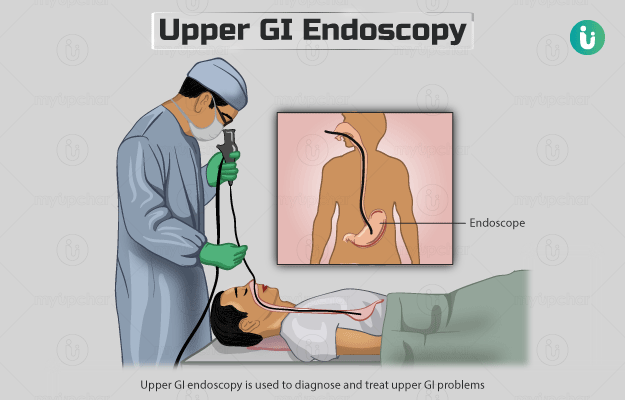
What is Upper GI Endoscopy?
Upper GI endoscopy, also referred to as gastroscopy or oesophagogastroduodenoscopy, is used to diagnose and treat upper GI problems. It helps your doctor to view the inside of your upper GI (or digestive) tract. The upper GI tract consists of the food pipe (oesophagus), stomach and the first part of the small intestine (duodenum).
This test is performed using an endoscope, which is a long, flexible tube with a tiny camera and a light attached at one end. The tube is inserted through the mouth into the oesophagus, stomach and duodenum. The video images captured by the camera can be viewed on a screen in real-time.
Read more: Why is an endoscopy done?