Summary
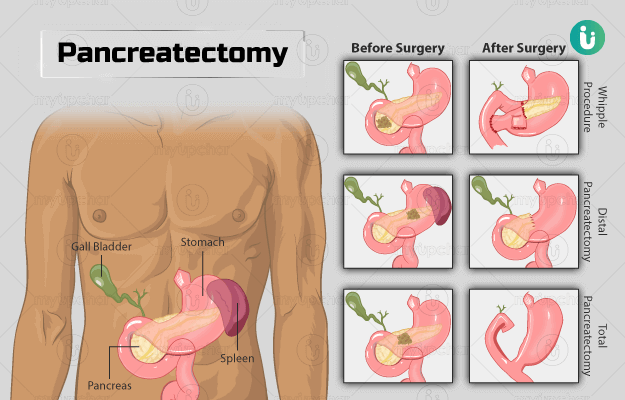
Pancreatectomy is a surgery to remove all or some portion of the pancreas, the abdominal organ responsible for producing insulin. This surgery is performed to treat pancreatic conditions, including pancreatic cancer. The various methods by which pancreatectomy is performed include Whipple procedure and distal and total pancreatectomy.
In this surgery, along with the pancreas, your spleen, gallbladder, and part of the stomach and small intestine may also be removed.
Before the surgery, medical tests are performed to check your overall health otherwise. You will need to fast for the surgery. Your doctor may ask you to quit smoking or stop alcohol before the surgery. The surgery is done under general anaesthesia. After the surgery, care should be taken to avoid strenuous activities. You may need to follow a high protein and carbohydrate diet. Avoid fat-rich food after surgery. A follow-up one to two weeks after the surgery is expected.