Summary
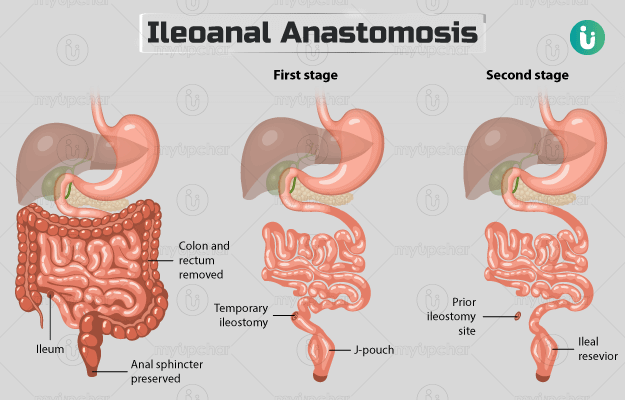
Ileoanal anastomosis is the surgical treatment for conditions like ulcerative colitis and familial adenomatous polyposis. During the surgery, the large intestine and rectum are removed, and the last section of the small intestine is connected to the anus. A temporary ileostomy will be formed until the intestine heals.
The procedure may take about two to four hours and may be performed by an open or laparoscopic technique. A hospital stay of about three to seven days will be needed after the surgery. Once at home, you may need to avoid spicy and fibre-rich foods and take care of the incision site until it heals. Your doctor may suggest you to avoid carrying weights during your recovery period, but you may be able to perform light exercises in moderation.
A follow-up will be scheduled about a week or two after the discharge, but you should call the doctor if you experience symptoms like fever and pain.