Summary
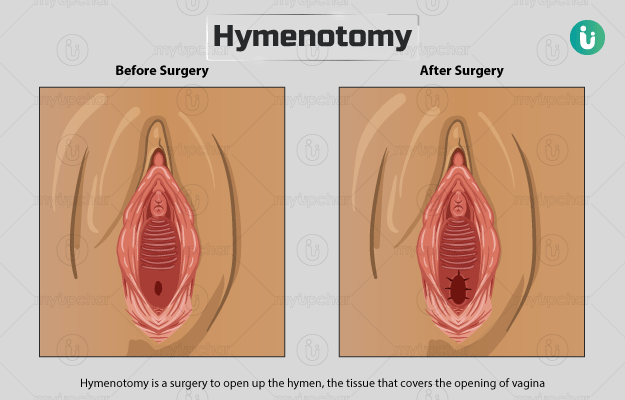
Hymen is a thin membrane that covers the opening of vagina but allows menstrual blood to flow out. Certain conditions of the hymen, such as an imperforate hymen, block the flow of blood during periods and lead to complications such as no menstruation, pain, and discomfort.
In such conditions, a hymenotomy is done to correct the problem and facilitate the passage of menstrual blood. At times, the procedure can cause complications like pelvic inflammatory disease or infection.