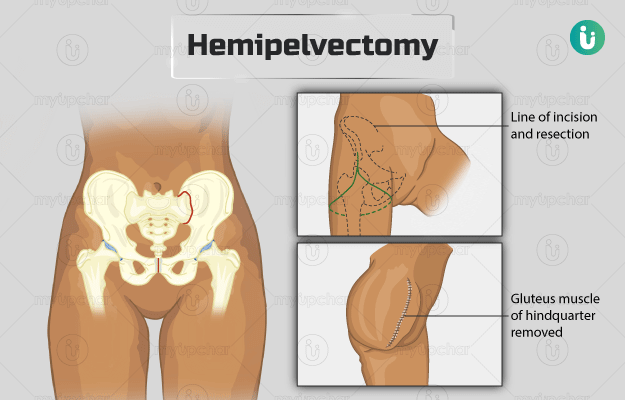
Hemipelvectomy is a complex surgery of the pelvis, that involves removal of the pelvic bone on one side, sometimes along with the limb on that side. It can be performed by external or internal technique. In external hemipelvectomy, half of the pelvic bone along with the leg on that side is amputated. In internal hemipelvectomy, the limb is preserved, and there is either complete or partial removal of the pelvis bone.
The hip bones form the bony structure of the pelvis along with two other bones (sacrum and coccyx), The pelvic cavity formed by these bones contains organs of the genitourinary tract such as the bladder and urethra, prostate gland and spermatic cords in males and uterus, fallopian tubes, ovaries, vagina and cervix in females; a large portion of the gastrointestinal tract; and nerves and blood vessels that supply to these organs and the limbs. During hemipelvectomy, it is necessary to identify and move these organs out of the way during the surgery to protect them.
This surgery is carried out in cases of tumours of the pelvic, hip, or thigh bone. It is performed to alleviate symptoms caused by uncontrollable malignancies or to prevent sepsis (the body’s reaction to infection leads to this life-threatening condition). A hemipelvectomy is also a treatment modality in cases of severe pelvic trauma.
Following surgery, the amputated part may be replaced with artificial prosthesis depending on factors such as age.
The best results from this surgical procedure can be achieved by a coordinated approach between various medical specialists such as surgeons, physiotherapists, occupational, and rehabilitative therapists.