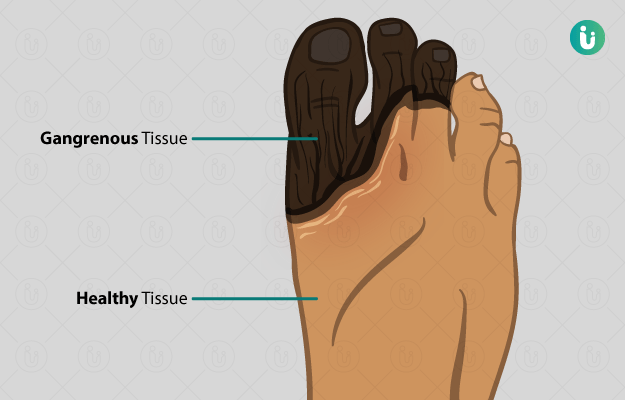
Gangrene refers to tissue death caused by inadequate blood supply or a severe bacterial infection. It is a serious condition and requires immediate medical attention. Gangrene most often affects the extremities, but it can happen anywhere, including internally. A serious injury such as a deep laceration or high impact blow that causes internal bleeding can lead to gangrene, or it can progress slowly due to clogged arteries or damaged blood vessels.
While serious injuries can lead to gangrene for anyone, those with underlying conditions involving the blood vessels are especially susceptible. These include atherosclerosis, Raynaud’s disease, peripheral artery disease and diabetes. Further, those who are obese, are smokers or have lower levels of immunity are also at a higher risk of gangrene.
Gangrene can be separated into dry and wet. Dry gangrene usually develops slowly and is caused by clogged vessels. Wet gangrene involves a bacterial infection in the necrotic (dead) tissue. Initially, symptoms include redness, loss of sensation or severe pain, and sores that may ooze a foul smelling discharge.
As gangrene progresses, the skin can turn a greenish black. If gangrene progresses even further into deep tissue and organs and also develops a bacterial infection, there may be severe pain, fever and overall distress.
In cases where gangrene is caught early, treatment is usually successful. Wet gangrene is more challenging to cure and will require a longer, more involved intervention. Many treatment options are available including debridement (removing dead tissue), antibiotic therapy, and hyperbaric oxygen therapy. (Read more: Oxygen therapy)
In more severe cases, amputation of the affected limb may be required, or reconstructive surgery using a skin graft may be needed as well. If the gangrene is caused by a blood vessel problem, surgery to patch the vessels may be required as well.

 Doctors for Gangrene
Doctors for Gangrene  OTC Medicines for Gangrene
OTC Medicines for Gangrene
 Gangrene articles
Gangrene articles
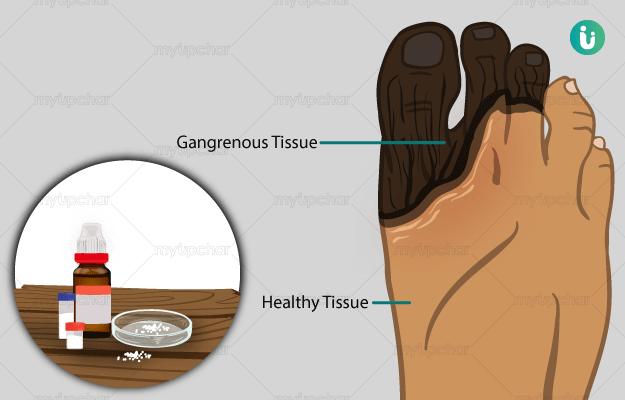
 Homeopathic Treatment of Gangrene
Homeopathic Treatment of Gangrene































 Dr. Rachita Narsaria
Dr. Rachita Narsaria











