Summary
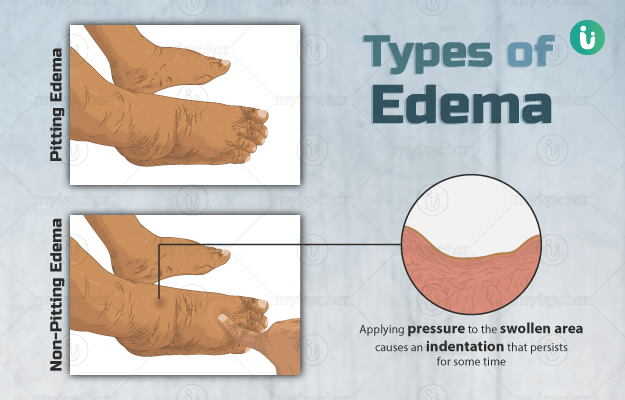
Oedema is a condition in which there is an excessive accumulation of fluid in the tissues of the body. It causes the skin over the swollen tissue to become warm, tender and stretched. Oedema usually involves the hands and feet (peripheral oedema), however, it may involve other parts of the body as well. The eyes and the tissues surrounding them are involved in conditions, such as papilledema and macular oedema, the abdomen in ascites, entire body in anasarca, skin and mucous membranes (usually of the throat, face, lips, and tongue) in angioedema, lungs in pulmonary oedema and brain in cerebral oedema. Peripheral oedema, which occurs in the hands and feet, commonly arises due to a defect in the blood circulation (venous insufficiency), congestive heart failure, kidney problems, a decrease in the blood serum proteins, liver disease, lung disorders and a damage to the lymphatic system (lymphedema).
Oedema involves one or both sides of the body depending upon the underlying health condition. Peripheral oedema is also common in women during pregnancy, menstrual cycle or periods, and following a long-term use of oral contraceptive pills. It is also common in people with long-standing anaemia and thyroid gland disorders. Certain medicines, such as antidepressants, calcium channel blockers (for high blood pressure) and steroids, also result in peripheral oedema. Depending upon the underlying cause, oedema may either last fora short duration or persist for along time. Treatment of the underlying cause is the first step in the management of oedema. Other measures include the use of stockings, weight-loss, keeping legs in an elevated position while lying down and adopting a salt-restricted diet.

 Doctors for Swelling (Edema)
Doctors for Swelling (Edema)  OTC Medicines for Swelling (Edema)
OTC Medicines for Swelling (Edema)
 Swelling (Edema) articles
Swelling (Edema) articles
 Ayurvedic Treatment of Swelling (Edema)
Ayurvedic Treatment of Swelling (Edema)
 Diet for Swelling (Edema)
Diet for Swelling (Edema)
 Homeopathic Treatment of Swelling (Edema)
Homeopathic Treatment of Swelling (Edema)





































 Dr. Rachita Narsaria
Dr. Rachita Narsaria

 Editorial Team
Editorial Team

 Dr. Laxmidutta Shukla
Dr. Laxmidutta Shukla