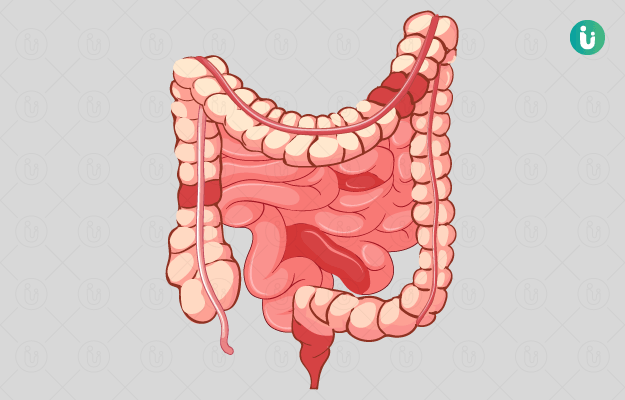
What is Crohn’s disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD). It is a chronic inflammatory condition of the digestive system and can affect any part from the mouth to the anus. It is a disease seen predominantly in developing countries and could be a result of urbanisation. The prevalence exceeds 0.3% globally. A comparative study showed that the incidence and prevalence were highest in India compared to other Asian countries.
What are its main signs and symptoms?
Primarily, Crohn's disease affects the lower segment of the small intestine. Signs and symptoms can be mild to severe and usually develop gradually, but can sometimes occur suddenly. Periods of remission can also occur where there are no apparent signs or symptoms. Symptoms which usually manifest when the disease is active are:
- Persistent diarrhoea
- Fever
- Fatigue
- Abdominal pain and cramping
- Bloody stools
- Sores in the mouth
- Poor appetite
- Weight loss
- Pain in the anal area due to fistula formation
Severe form of Crohn’s disease may show:
- Inflammation of the eye, joints and skin
- Inflammation of the hepatic or biliary ducts
- Delayed growth or sexual development in children
What are its main causes?
It affects men and women equally and is commonly seen among people in the age group of 15-35 years. There is no specific cause responsible for Crohn’s disease. Some factors are likely to increase the risk of the disease:
- Heredity: Individuals with a family history of Crohn’s disease are at higher risk.
- Immune system: It has been suggested that a virus or bacterium may trigger an abnormal immune-mediated response which causes the immune system to attack the cells in the digestive tract, causing inflammation.
- Environmental factors like living in an urban area and a diet rich in fat and refined foods may also play a huge role.
- The risk is higher in people of Eastern European descent.
How is it diagnosed and treated?
Some common tests which are usually performed include:
- Blood tests:
- Imaging tests:
- Standard and contrast X-ray
- Computed tomography (CT) scan
- Leucocyte scintigraphy
- Endoscopy
- Magnetic resonance imaging (MRI)
Treatment mainly focuses on the use of medicines, dietary changes and sometimes surgery to remove the affected part.
- Medications that suppress the immune system and reduce inflammation are usually prescribed. An immunomodulator may be used in combination with an anti-inflammatory agent.
- Since the appetite is poor in this condition, dietary modifications can help in having a balanced diet. Eating bland foods instead of spicy, oily and fibre-rich foods may help in reducing inflammation.
- Surgery is considered an effective non-drug treatment option. Nearly 70% of patients might eventually need surgery.
Self-care and follow-up measures:
- Make a list of all prescribed and over-the-counter (OTC) medicines that you take. This can help you and your doctor to know more about your condition and help in preparing a customised treatment plan for you.
- Avoid non-steroidal anti-inflammatory drugs, as it can worsen the condition. If you need to take them, do consult with your physician first.
- Avoid regular intake of spicy foods, as this can increase your discomfort.
- Track your symptoms and note it down.
- Go for regular follow-up visits.

 Doctors for Crohn's Disease
Doctors for Crohn's Disease  OTC Medicines for Crohn's Disease
OTC Medicines for Crohn's Disease