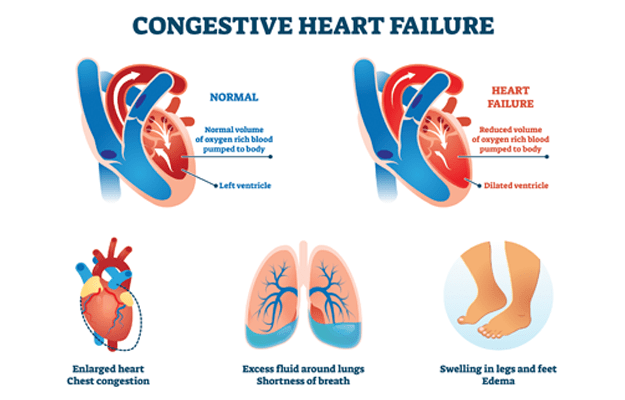
Congestive heart failure (CHF) is a medical condition in which a person’s heart is unable to fill completely and pump out blood effectively with each heartbeat due to failure of heart function. Contrary to what it may sound like, congestive heart failure or congestive cardiac failure (CCF) does not mean that the heart has stopped or it is going to. It is also important to note that congestive heart failure (CHF) is not the same as a ‘heart attack’, the common name used for myocardial infarction, in which a part of the heart tissue dies due to a clot in the coronary arteries supplying oxygen to the heart. Nor is congestive heart failure (CHF) the same as a cardiac arrest, in which there is a sudden loss of blood flow to the body due to complete failure of the heart’s pumping mechanism.
Please click on this link to know better about heart disease treatment.
As a result of the heart being unable to maintain the required pressure to pump out enough blood forcefully with each heartbeat in congestive heart failure, the blood circulation of the body falters, producing typical symptoms that include shortness of breath, swelling in the legs and tiredness. Not all congestive heart failures are equally disabling; the severity of the condition is usually tested by breathlessness experienced on exertion after exercise. Any health condition that alters the function or structure of the heart can result in congestive heart failure (CHF).
(Read More - Enlarged Heart Treatment)

 Doctors for Congestive Heart Failure (CHF)
Doctors for Congestive Heart Failure (CHF)  OTC Medicines for Congestive Heart Failure (CHF)
OTC Medicines for Congestive Heart Failure (CHF)