Melasma is a skin condition in which brown or greyish-brown spots appear on the face—especially the nose, cheeks and forehead. The spots may also appear on the neck, shoulders and forearms.
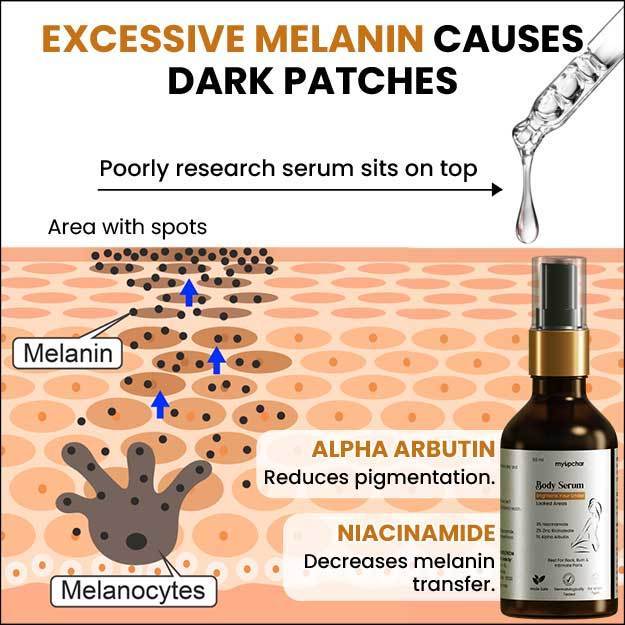
Melasma is a skin pigmentation disorder. Though scientists don’t know its exact cause, they suspect the involvement of melanocytes or cells that make melanin—the pigment which gives our skin and hair their colour.
Anyone of any age can get melasma. That said, some groups that are at a heightened risk for melasma are pregnant women and people with darker skin. Women, in general, are much more likely to get melasma than men.
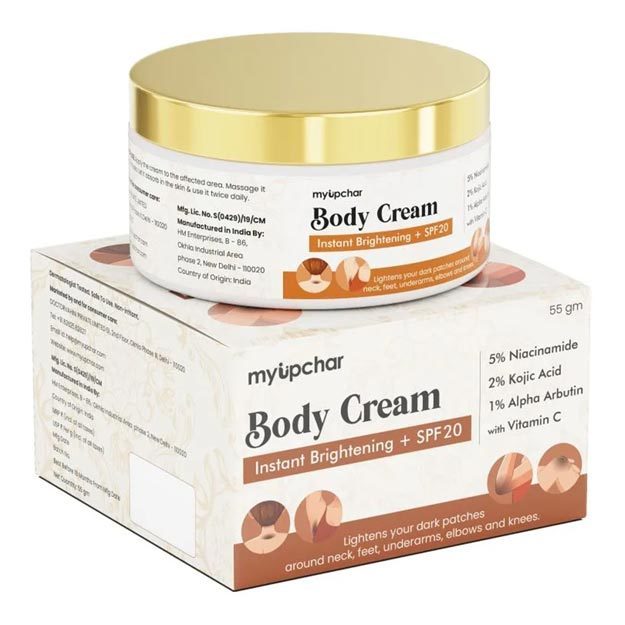
Research shows that exposure to the sun’s ultraviolet rays can trigger or worsen melasma spots. Therefore wearing the right sunscreen for your climate and needs is one way to prevent or contain these spots.
So far there’s no evidence to suggest that melasma could be harmful, though some people may not like the spots on their face and upper body from an aesthetic point of view.
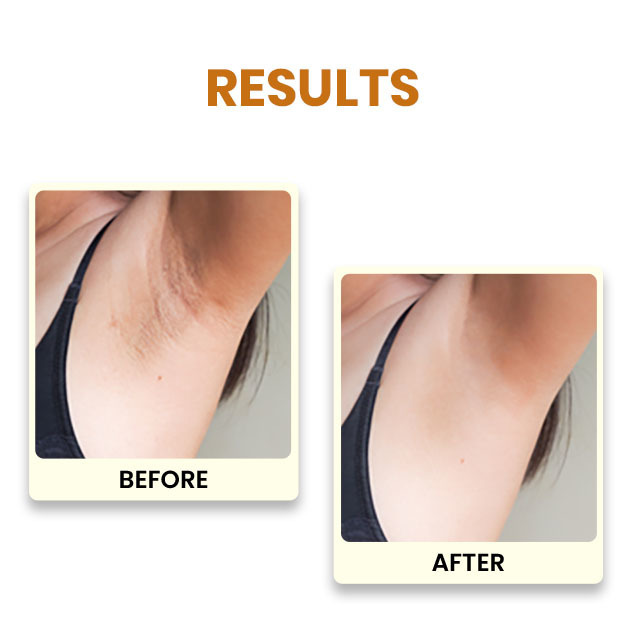
In some cases, melasma spots go away on their own. For example, in most cases, melasma in pregnancy resolves on its own after delivery. In cases where the melasma pigmentation disorder persists, patients can seek optional treatments like topical application of hydroquinone, chemical peels and microdermabrasion to lighten or remove the spots—at least temporarily.
Melasma is quite common in India; indeed, in Asia. Read on to know more about the symptoms, causes and risk factors, prevention, diagnosis and treatment of melasma.