Summary
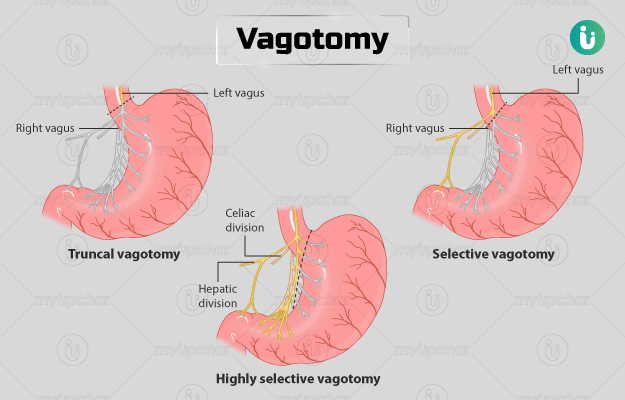
Vagotomy is a surgical procedure that involves cutting the vagus nerve - the nerve that controls the secretion of stomach acid. The procedure is done for the management of peptic ulcers in patients who present with symptoms such as nausea, vomiting, weight loss, loss of appetite, black or bloody stools, or pain and burning sensation in the stomach, that cannot be relieved with any medical treatment. You will need to fast from midnight before the day of the surgery. Tell your doctor before the surgery if you have an allergy, if you smoke or are pregnant. After the surgery, you will need a follow-up appointment to check your health.