Summary
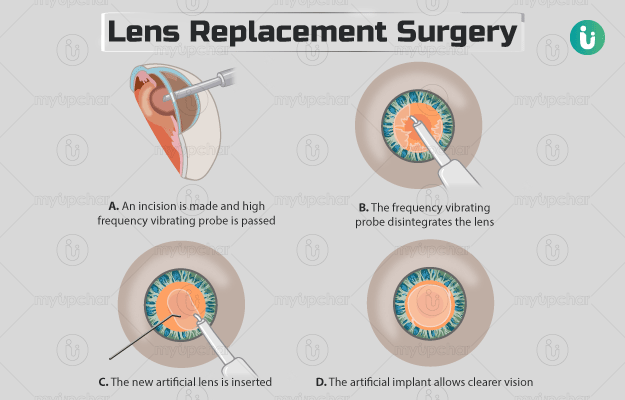
Lens replacement surgery involves the replacement of the natural lens in the eye with an artificial lens. This surgery is performed to provide sharpness of vision and reduce the need for glasses or contact lenses. The surgeon will choose a lens based on the purpose of the operation. For example, if you need to reduce the dependency of spectacles for distant vision, the doctor may suggest a monofocal lens. Similarly, a multifocal lens will serve your purpose for near vision. Before the surgery, your ophthalmologist will examine your eyes and measure them to ensure that you get the correct lens for your eyes. The surgery will be done under local anaesthesia. After the procedure, a nurse will cover your eyes with a protective shield. Once you are discharged, make sure to follow the instructions given by the doctor for a speedy recovery.