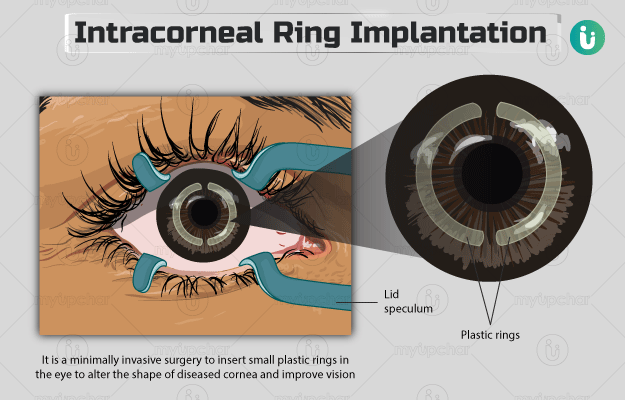
Intracorneal ring segment (ICRS) implantation is a minimally invasive eye surgery that involves the implantation of a medical device into the cornea to alter its shape and improve vision.
Cornea is the strong, transparent, outermost tissue of the eye. Apart from protecting the eye from dust, germs, and other foreign substances, it plays an important role in vision. Cornea acts like a window that controls the light entering the eye. When light rays reflecting from an object reach the cornea, it bends the light and focuses it onto the eye’s natural lens. The lens then projects the light onto the retina that converts this light into impulses, which are moved to the brain through the optic nerve. Therefore, the refractive function of the cornea is essential for vision.
However, in certain eye conditions such as keratoconus, cornea loses its natural shape and becomes thinner and steeper, resulting in progressive vision loss. Although the condition can be initially treated with contact lenses or glasses, it may worsen with time, requiring the individual to undergo corneal transplantation.
Intracorneal ring segment implant provides an alternative to corneal transplantation. The surgery includes placing two small, crescent-shaped plastic rings into the cornea to restore its natural shape.
ICRS implantation is better than corneal transplantation because the rings can be easily removed if any complications arise.
The surgery does not treat keratoconus and, therefore, it is generally combined with another procedure called corneal collagen crosslinking to make the cornea stable.