The surgery takes place in the operation theatre. Before the surgery:
- The doctor will place a needle in your vein to give you sedatives or any medicines if required during surgery.
- He/she will sterilise the region around the affected eye and cover your face with drapes such that only the eye region is visible.
- You will then be given anaesthetic intravenously. This will help you relax.
- The surgeon will give an injection around your eye to numb the area. The procedure is performed under local (the surgical area is made numb) or general (person is made to fall asleep) anaesthesia.
- You will be asked to keep your head still and lie down flat for the duration of the surgery.
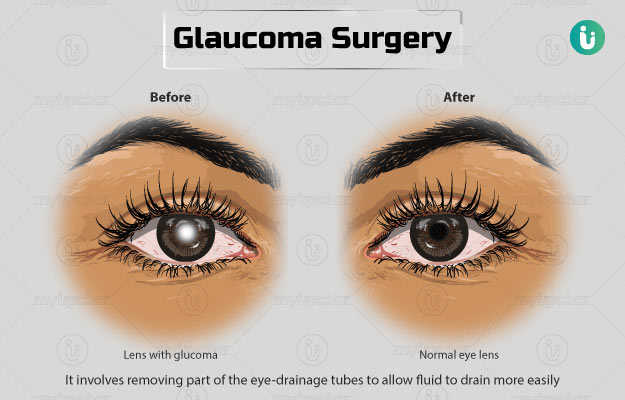
The main types of glaucoma surgeries and their procedures are as follows:
Trabeculectomy
The aim of this surgery is to allow the fluids from within the eye to come out through its walls and under the tissue that covers the eye (conjunctiva), from where they can be absorbed.
- The doctor will use a binocular microscope to look at your eye during the surgery.
- He/she will make a cut to your conjunctiva and fold it back. Next, a cut will be made to your sclera (white part of the eye) and a flap will be created. This flap will be folded backwards, and a few bits of the scleral tissue will be removed to create a cavity within the front compartment of the eye.
- The surgeon will also remove a part of your iris from under the cavity.
- Then, he/she will stretch the flap over the cavity and stitch it using nylon sutures. The sutures act as a valve to control the flow of the aqueous humour and prevent it from leaking out entirely.
- Finally, the surgeon will stitch your conjunctiva to its original position so it covers the sclera. The conjunctiva begins absorbing the fluid that comes out.
- The sutures may be loosened after the surgery to make adjustments in the eye pressure. Therefore, releasable stitches are used.
- The surgeon will cover your eye with an eye pad or shield.
In order to keep the flap functioning like a valve and prevent it from healing itself, anti-healing medication like mitomycin-C or 5-fluorouracil will be used in the eye during the surgery.
On an average, this procedure takes an hour to complete.
Tube-shunt surgery (implant surgery)
Tube-shunt surgery has the same purpose as of trabeculectomy but is carried out in cases where a scar is formed in the surgical area from an earlier surgery. This surgery is preferred in cases of eye inflammation, secondary glaucoma and in some children with glaucoma.
- The surgeon will make an incision and insert a tiny flexible plastic tube with a flat base into the front chamber of your eye. The tube will be extended to the back of your eye, where its flat base is sewn to the sclera of the eye.
- This tube will collect the aqueous fluid. This fluid then gets absorbed into the cavity created near the plastic base.
- In order to prevent the IOP from dropping too low shortly after surgery, the surgeon will stitch the opening of the tube. The stitches will dissolve on their own in about five weeks of surgery.
- This procedure takes around one to two hours to get complete.
Laser ciliodestruction
Laser treatment helps reduce the quantity of aqueous humour released by the ciliary body (the circular-shaped structure that extends from the iris, the coloured portion of the eye) by burning the ciliary structures.
- In this procedure, the surgeon will treat more than half the ciliary body structure of your eye with a laser to lower the fluid generated to a manageable level, but not entirely stop it.
- The surgeon may focus the laser beam in your eye using a special probe. The probe will pass the beam (from outside your eye) through the surface of your eye along a fiber optic cable. Alternatively, a laser beam may be delivered by inserting the probe directly in the front of your eye.
- The approach from the outside of the eye is followed when trabeculectomy and tube shunting have failed.
Minimally invasive glaucoma surgeries:
- Trabectome: The procedure improves the release of aqueous fluid and reduces pressure by taking out a fine layer of the trabecular tissue.
- Canaloplasty and gonioscopy-assisted transluminal trabeculectomy (GATT): These work by opening up the drainage canals through which the fluid leaves the eye.
- iStent: This surgery introduces small metal tubes in the trabecular meshwork of the eye to improve drainage.
You will be allowed to go home on the same day. The next day, your eye will be assessed to ensure that the fluid drains appropriately and the IOP is lowered. The eye pad should be kept in place for a day after surgery.