Summary
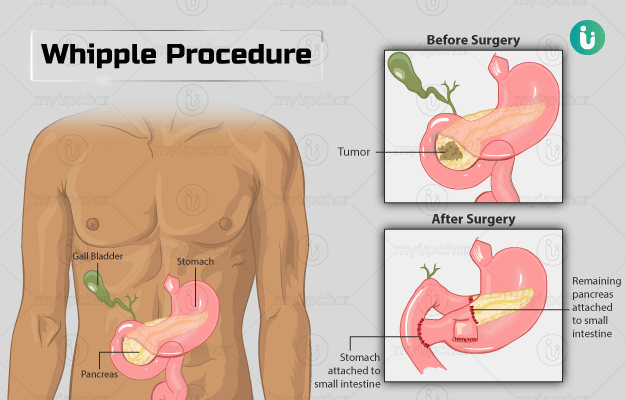
The Whipple procedure is performed for the treatment of pancreatic cancer. The pancreas plays an important role in digestion and blood sugar level regulation; however, these functions are hampered when a tumour develops in pancreas.
Whipple procedure can also be done for small intestinal or bile duct cancer and chronic pancreatitis. However, it is not performed if the cancer has spread.
The surgery involves the removal of the head of the pancreas, gallbladder, portion of the bile duct and small intestine, and in some cases, a section of the stomach. The remaining organs are reconnected so that the digestive system can continue to function. The procedure is performed under general anaesthesia. You will need a hospital stay of about two weeks. Visit the doctor immediately if you observe any symptoms such as pain, swelling, and redness at the incision and fever. Your follow-up visit will be about two weeks after your discharge.