Summary
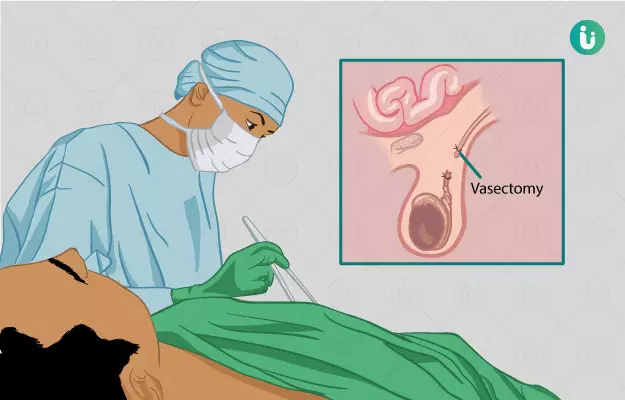
Vasectomy, also called male sterilisation, is performed to provide a permanent means of birth control to couples. In this procedure, a man’s vas deferens (the tubes that carry sperms) are either sealed or cut off. This procedure is 99.99% effective and even though vasectomy is said to be reversible, the surgery for reversal is complicated and is not always successful. So only opt for it if you are sure that you do not want to have a child.
Vasectomy is either performed in a surgeon’s clinic or in an outpatient centre. You will usually be discharged on the same day of surgery. You may require 7 to 9 days for complete recovery. After the surgery, you would need to visit the clinic once or more than once for semen analysis to make sure that your semen contains no sperm.