Summary
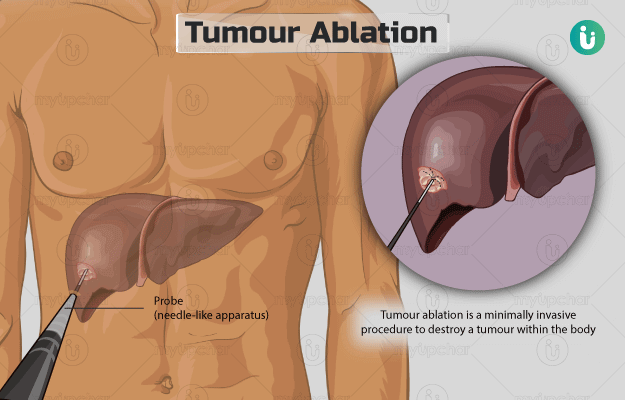
Tumour ablation is a minimally invasive procedure to destroy a tumour within the body without the need for open surgery. This is achieved by inserting a probe (needle-like apparatus) into the body through a small incision (cut) made on the skin. The probe is guided towards the tumour using imaging procedures such as ultrasound, magnetic resonance imaging (MRI), or computer tomography (CT) scan. Once the probe is within the tumour, it subjects the diseased tissue to electric current, heat, low temperature, or chemical to destroy it. The procedure lasts for around two hours, and you will be able to go home after an overnight stay at the hospital.