Summary
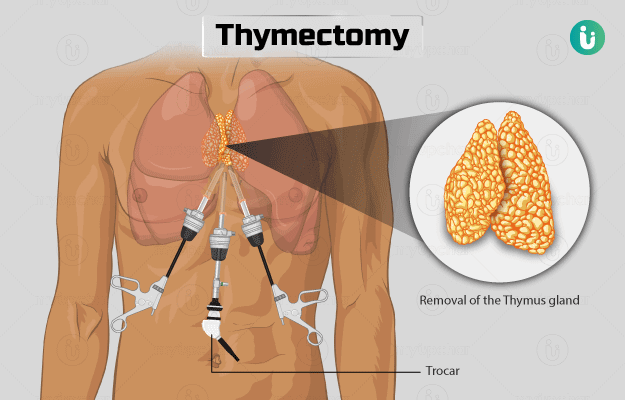
Removal of the thymus gland is known as thymectomy. The thymus gland is located inside the chest cavity and is active during infancy and early childhood stage. It is responsible for the development of the immune system. Later, when puberty hits, this gland shrinks. Thymus gland does not have a role in immunity development in adults.
Thymectomy is performed for two conditions, namely myasthenia gravis and thymoma (a thymus tumour). Recovery after the surgery depends on the type of surgery performed and may take a few weeks. You may need to follow-up with your doctor six weeks after the surgery.