Summary
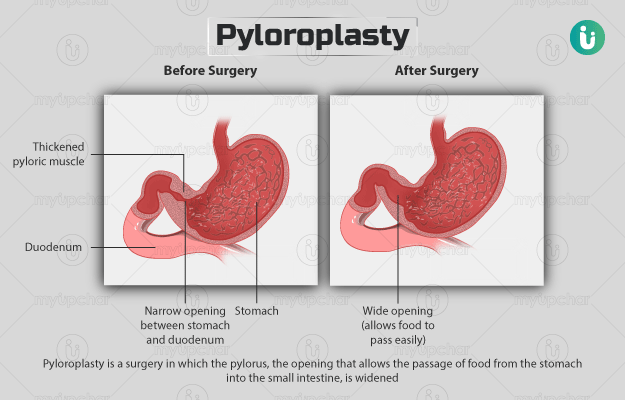
Pyloroplasty is a surgery in which the pylorus, the opening that allows the passage of food from the stomach into the small intestine, is widened. The surgery is performed in individuals with conditions such as peptic ulcer and gastroparesis that cause narrowing of the pylorus and blockage of food. Pyloroplasty is performed under general anaesthesia, you will be in a deep sleep for the duration of the surgery. During the surgery, after the pylorus is accessed, the wall of the pylorus is cut and stitched together such that the opening is widened. The surgery takes one to two hours. After the surgery, you may have to stay in the hospital for one to three days or until your condition is stable.