Summary
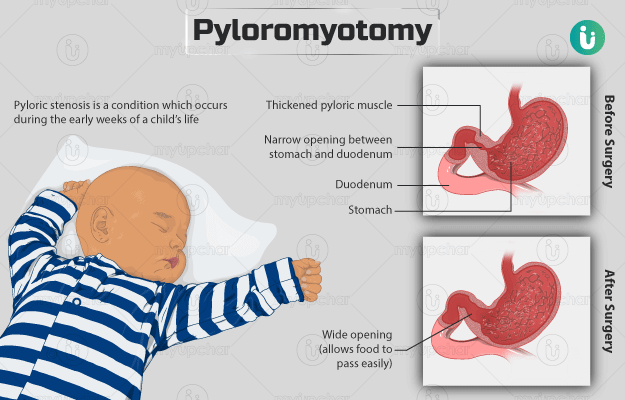
Pyloromyotomy is a surgical procedure that is performed for the permanent management of pyloric stenosis in infants. Pyloric stenosis is a condition wherein the muscle fibres around the opening of the stomach into the intestine (pylorus) become abnormally thickened, resulting in the narrowing of the opening. This condition prevents the passage of food into the intestines, which causes the infant to vomit after each feed.
The surgeon approaches the pylorus either by open surgery, which requires one large incision, or by laparoscopic surgery, which requires two to three tiny incisions. Laparoscopic surgery is generally the preferred method of surgery. The child will go into a deep sleep (achieved via the administration of anaesthesia) throughout the procedure. Some of the complications specific to this surgery include vomiting, a hole in the stomach wall and hernia at the operated site. Post-surgery care requires the child to stay at the hospital for about two to four days. Pyloromyotomy helps in successfully reducing or stopping the incidence of vomiting after meals.