There are two types of pneumonectomy: traditional and extrapleural pneumonectomy. Traditional pneumonectomy usually involves the following steps:
- You will be asked to lie on your side with the arm on the side to be operated on placed over your head.
- The medical staff will insert an intravenous line into your arm, through which medicines and fluids will be given.
- The anesthesiologist will then give you general anaesthesia to make you fall asleep.
- The surgeon will make a long incision between your two ribs over the diseased lung. The incision will extend from under your arm to the back.
- Next, the surgeon will separate your ribs; in some cases, a small portion of the rib will also be removed.
- He/she will clamp the bronchi (the branches of the windpipe supplying air) to the diseased lung and tie off the blood vessels that supply and drain blood to and from the diseased lung. The blood vessels will be moved away from the area of surgery.
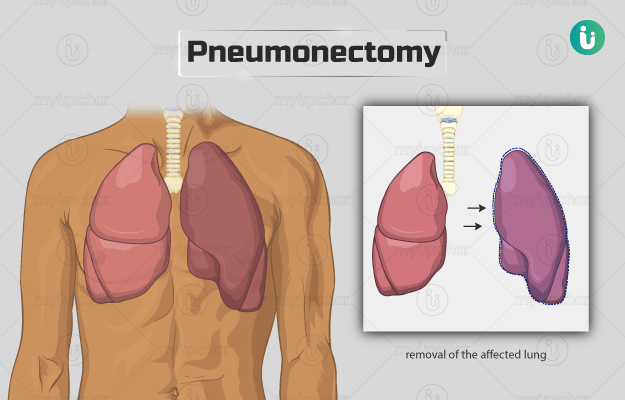
- Then, the surgeon will deflate (collapsed) and remove the affected lung.
- He/she will bring your ribs back in their original position, close the muscles and skin over it and cover the incision with a dressing.
Finally, the surgeon will insert a tube into the operated area of your chest. This tube is temporary and will be removed when your condition becomes stable.
In extrapleural pneumonectomy, parts of diaphragm and pericardium and the lining of the chest cavity are also removed along with the lung and will be replaced with a safe, synthetic material.
The surgery can also be performed by a minimally invasive method known as video-assisted thoracoscopic surgery. In this procedure, the surgeon makes several tiny cuts instead of one large cut. Several instruments are inserted through the cuts, including a thoracoscope (a special instrument containing a video camera), to remove the affected lung.
After the surgery, the hospital staff will wheel you to an intensive care unit where an external device will assist you in breathing for the first 24 hours. Once your condition is stable, you will be moved to a regular hospital ward. Individuals who have undergone traditional pneumonectomy need to be in the hospital for seven days, while those who have undergone extrapleural pneumonectomy have to be hospitalised for eight to nine days. You can expect the following after surgery:
- You may be in a state of confusion when you wake up. This is due to the effects of the anaesthesia which will soon wear off.
- A nurse will monitor your vital signs, such as oxygen level, blood pressure, breathing and heart rate are continuously monitored.
- You will be given pain medicines for any pain you may feel at the operated area.
- You will be given oxygen through an oxygen mask and your urine will be drained through a tube (catheter) in your bladder.
- You may also be provided with special stockings to prevent the formation of blood clots in your legs.
- The medical staff will teach you special breathing techniques, which you should do several times a day to keep your airways open.