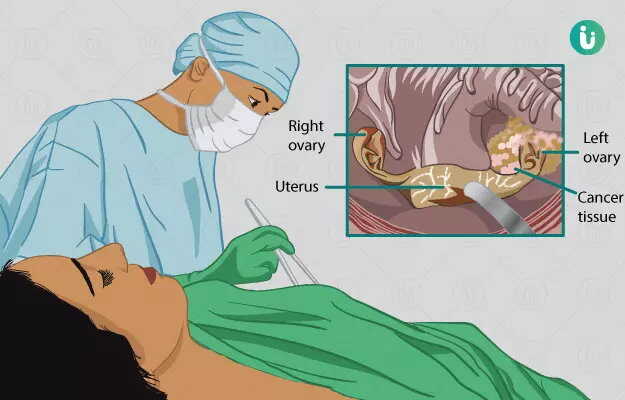
Oophorectomy is a surgical procedure where one or both ovaries are removed. It is required in pathological conditions related to the ovary where medical management has a limited role.
The surgery, if it includes removal of both ovaries, develops infertility and menopause. Hence, appropriate counselling for the patient is required before going through with the surgery. Investigations usually include blood tests and radiological tests.
The duration of the surgery and hospital stay afterwards depends upon the technique employed and the nature of the disease. Postoperative recovery varies from two to six weeks.