Summary
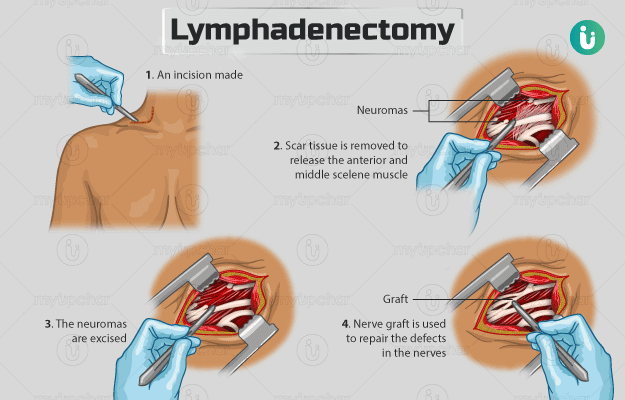
Lymphadenectomy is the surgical removal of a lymph node or nodes (from particular regions of the body) that are susceptible to cancer or are already affected by it. Lymph nodes are a part of the lymphatic system and are present throughout the body. They act as a line of defence for the body and help fight infections. However, cancer can spread from one location to the other through lymph fluid - the fluid that flows through lymphatic system.
Lymph node removal is preceded by sentinel lymph node biopsy. This step evaluates if the first lymph node that drains lymph from the tumour is affected by the cancer. As lymph nodes are present all around the body, lymphadenectomy may be carried out wherever cancer has spread, for example, the lungs, cervix, abdomen and armpits. Lymph node removal can be performed by simple or laparoscopic approaches.