Once you are in the hospital, you will be given a hospital gown to wear. A nurse will give you special stockings or medicines to prevent blood clot formation in your legs. The medical staff will place an intravenous (IV) line in your arm to administer essential fluids and medicines during the surgery.
You will then be taken to the operating room where you will lie on a medical table. Different devices will be attached to you to detect your vitals, including your heart rate, oxygen levels, and blood pressure. The surgery is performed with general anaesthesia (a sleep-inducing medicine). After you fall asleep, a catheter (tube) will be inserted into your bladder to remove urine.
Longitudinal pancreaticojejunostomy may be performed by open, laparoscopic, or robotic methods.
The following steps are performed for open surgery:
- The surgeon will make a straight or curved incision (cut) on your abdomen.
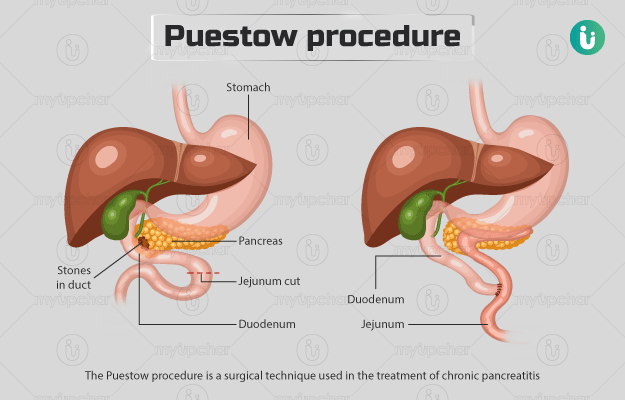
- He/she will examine your stomach and duodenum for ulcers and your gallbladder for stones.
- Next, the surgeon will lift up your duodenum to examine the head of your pancreas.
- He/she will place a cut along your pancreatic duct to divide the duct but leave the tip of the pancreatic tail.
- Next, the surgeon will remove any stones that may be present in your pancreatic duct.
- He/she will make a long cut on your jejunum and connect the divided pancreatic duct to the opening in the jejunum with the help of sutures (anastomosis).
- The surgeon will then place drainage tubes near the pancreaticojejunostomy, close the abdominal tissue with stitches and the incision with staples.
In a laparoscopic procedure, a few small cuts are made (instead of one large cut) on the abdomen. Through one of these cuts, the surgeon passes a tube with a camera to view the internal structures, and through the other openings, special tools are inserted to perform the surgery.
Robotic surgery is an advancement to laparoscopic surgery, in that, it is done with special robotic tools that move the equipment and perform the surgery, and the viewing of the internal organs is magnified and three dimensional.
The surgery takes about two and a half hours. Once the procedure is over, the medical staff will move you to the recovery room and monitor your vital signs. When you wake up, you may feel pain, for which the nurse may provide medication. You will be asked to perform chest and lung exercises and encouraged to walk around after the surgery. You will need to take pancreatic enzyme therapy and get checked for diabetes. The catheter will be taken out after two days.
Initially, you will be given fluids through the IV, on the third day after the surgery, you will be able to eat food, and over the next few days, you will be able to take your regular diet. You will be discharged from the hospital after five days.