Summary
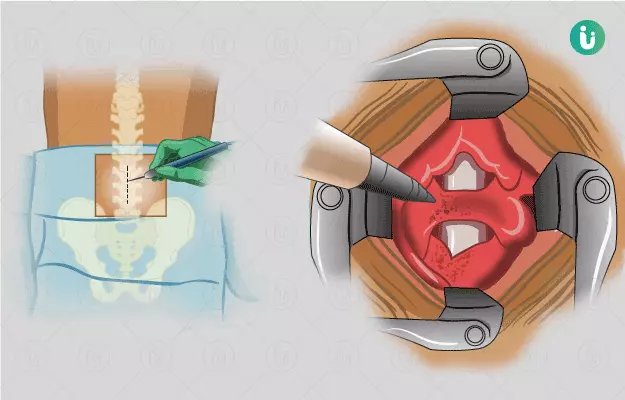
Laminectomy is a surgery performed to remove the lamina (plates of bones on the posterior part of the spinal column) to alleviate the pressure on the spinal cord, which may have been caused by an injury, infection, tumour, or other bone conditions of the spinal column. Before the surgery, the doctor may perform some blood tests and imaging tests. The surgery is usually performed under anaesthesia and can take about 1 to 3 hours. You may need to stay in the hospital for up to 3 days. However, recovery may take longer, about 6 months to 1 year. You may have to visit the surgeon for follow-up 2 to 3 weeks after surgery for the removal of sutures or staples.