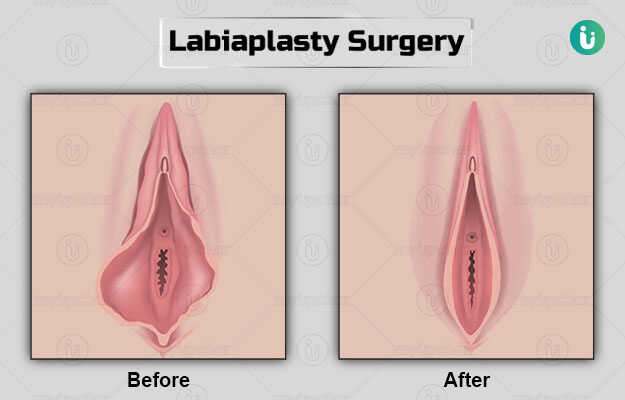
Labiaplasty is a surgical procedure done to alter the size of the labia minora or/and labia majora (the skin folds that surround the urethra and vagina).
The reason for surgery is either cosmetic or medical-related.
Preoperative counselling regarding the reason for surgery is important. Prior to surgery routine blood tests are required.
The procedure is mostly a daycare admission but may require further hospital stay depending on the complexity of the surgery.
Aftercare involves taking care of the wound to prevent further bleeding or injury to the wound. Complete healing takes about 4 to 6 months.