Summary
The main role of the kidneys is to filter out waste from our blood through urine. Any injury to or disease of the kidneys may affect their normal function leading to the buildup of toxins in the blood, which can be life-threatening if not managed in time.
When the kidneys fail, the most commonly employed treatment is dialysis, wherein artificial blood filtration is done using a machine that mimics kidney structure in a hospital setting. The second method, which is known as kidney/renal transplant, is the replacement of the failed kidney by a fresh one taken from a suitable donor. In this surgery. Getting a donor is crucial and it mostly takes a long time to find one. Thus, you are kept on a waiting list and as soon as a donor is available, you'll get the transplant done. It is usually placed on the right side. A few short-term and long-term risks are associated with a kidney transplant, which is discussed in the article.
It is estimated that more than 3500 people undergo this operation in India each year. According to the Indian transplant registry, a total of 20952 kidney transplant operations have been performed in 48 hospitals over the years. However, access to this surgery and availability of suitable donors is difficult in a country like India.
- What is a kidney transplant surgery
- Why is kidney transplant surgery done
- Preparations before kidney transplant surgery
- How is kidney transplant done
- Post surgical care
- Risks and complications of kidney transplant surgery
- Things to take care of while recovering
- Outcome of kidney transplant surgery
- Follow-up and support
What is a kidney transplant surgery
A kidney transplant surgery is usually done to replace a damaged kidney with a new one from a healthy donor in order to maintain body fluid and electrolyte balance. It is the most commonly carried out transplant operation around the world.
Renal replacement is carried out in 200 centres in India, which majorly depends on the availability of ‘alive donors’ (usually relatives).
The cost for this surgery ranges between 5 lac in a government hospital to 30 lac in the private sector with the average cost for maintenance after surgery being Rs 1,20,000/year for medications and follow-up.
Why is kidney transplant surgery done
Kidney transplantation is the treatment of choice in case of kidney failure. This operation is considered beneficial in prolonging survival and improvement in the quality of life of people with end-stage kidney disease as compared to dialysis. Other causes of damage to kidneys include:
- Uncontrolled diabetes.
- High blood pressure.
- Blood vessel blockage.
- Birth defects.
- Immune system diseases, where the body's own defence mechanism attacks its organs and causes damage.
Preparations before kidney transplant surgery
Speaking to nephrologist
After the diagnosis, you will visit a nephrologist (Kidney specialist) to check your fitness for a transplant. Initially, questions regarding financial ability will be asked and important information will be provided to you and your family members. This is to ensure that you are aware of the expenses and details of the treatment beforehand. If you are already on dialysis then your dialysis team will work together with your doctors throughout the transplant stages.
Getting tested
You will undergo multiple sets of tests long before your preparation for the operation. It’s a time-consuming process (takes months) and usually takes place in an out-patient setting. Your reports will be thoroughly reviewed, analysed, and discussed to ensure there are no potential complications, during or after the procedure.
These tests are done to rule out any obstructions to successful transplant surgery. The tests include:
- ECG for heart diseases
- Chest X-ray for lung disease
- Liver function test
- Substance abuse (alcohol, tobacco, or drugs) test.
- Tests to identify conditions like HIV, cancer, Hepatitis B, TB, obesity, any immune system diseases, uncontrolled high blood pressure, smoking and other mental health issues may also be conducted.
Finding a donor
Finding a donor is the most difficult yet crucial stage to get a kidney transplant done. Two types of donors may be chosen:
- Living Donor
You may either have a friend or a family member who might be willing to donate a kidney and are potentially a good match. They will have to undergo a similar, lengthy health examination to make sure they are fit for donation. - Deceased Donor
A deceased donor is a person who has just died (brain dead) for example, a healthy donor who was taken off the life support system or had a sudden death.
Waiting List
Once your tests indicate you are fit for the transplant, your name will be added to a waiting list for getting the organs from deceased donors if living donors are not available.
In a process called “cross-matching”, your doctor will test the blood from the donor against your blood to predict your immune system’s acceptance of the organ from the donor and avoid transplant rejection.
Meeting the transplant team
A team of surgeons, nephrologists, nurses, social workers, nutritionists and financial coordinators will foresee your treatment and adequate medical care. This will be coordinated by a transplant coordinator who will follow up on your referrals, reports and clinical findings by the team.
To ensure you have a thorough knowledge of the entire procedure, do speak to your doctor and clear your doubts and get answers to all your queries.
Preparations right before surgery
Certain instructions will be given to you by your nurse/doctor, which you must follow before the operation, such as stopping or taking certain medication, coming empty stomach, quitting alcohol and tobacco consumption, foods to include in your diet, things to bring to the hospital and so on.
Testing before the operation is an essential part of the preparation for the surgery, which might include evaluation of your status of health, medical history and circumstances at home.
- Medical examination
A detailed history of your medications, supplements, full body check up and a few laboratory tests will be done before the day of your operation. You will be asked to stop eating or drinking (this is to ensure you do not vomit while you are under general anaesthesia) and stop any medication a few hours before surgery. - Consent
Final consent for surgery and of your knowledge about the risks will be taken prior to the surgery from you or your family member. - On the day of surgery
On the day of surgery, you will be given a clean surgical gown/clothes. In the operation theatre, your blood pressure, blood oxygen levels, airway, and heart rate will be monitored.
You will be covered with a germ-free cloth and the site of operation (your belly) will be cleaned with an antiseptic/ antibacterial medicine or solution. This is to ensure proper hygiene and germ-free environment at all times during the operation.
How is kidney transplant done
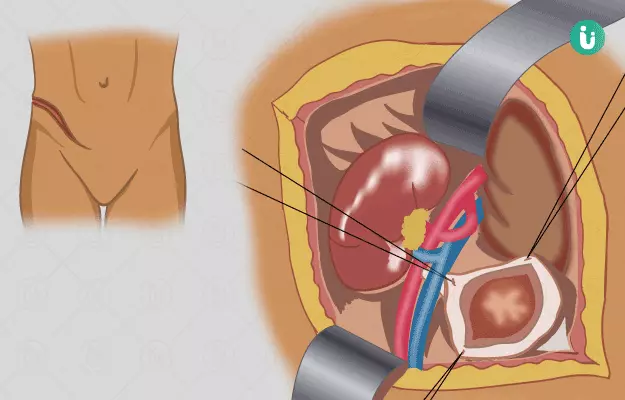
This operation was initially done using an ‘open surgery technique”. In recent years, a closed and common technique using ‘laparoscopy’ and robotic machines has evolved. A small cut is made using the latter approach.
Steps of the procedure:
A numbing agent will be injected into your blood through a drip placed in a blood vessel of your hand after you inhale a sedative. A specialist from the anaesthesia team will be available throughout your operation.
- Open donor nephrectomy
This involves surgical removal of the kidney from the donor’s body. Although, it is rarely done nowadays but is carried out under general anaesthesia in which you sleep during the surgery under the effect of the numbing agent. - Laparoscopic donor nephrectomy
In this step, a wand-like camera will be inserted into a small cut made in your belly, and the kidney will be safely removed. - Transplantation
Finally, the surgeon will proceed into the hollow space beneath your small intestine (ilium) on the right side, which is considered the ideal space for a kidney transplant. The transplant procedure involves 3 stages:- A cut made in the lower belly through which the donor kidney will be put in place. Your own kidneys will be left at their original place as long as they are not causing a problem.
- The major blood vessels will be attached to the donated kidney to ensure blood supply to the organ for its functioning.
- Finally, the ureter or the tube connecting the kidney to the bladder will be reattached.
- A plastic tube, known as a stent, may be inserted from the opening of the ureter to ensure good urine flow and will be removed within 6 to 12 weeks. This is called ‘cystoscopy’. Now, the cut will be closed using stitches and tapes.
Post surgical care
After a successful operation, once the effect of anaesthesia will wards off, you will feel dizzy and nauseous for a while and slowly you will regain consciousness in the recovery room. You will be shifted to an ‘intensive care unit’ for observation to ensure no complications arise in the next 24-48 hours. If the transplant was carried out from a live donor, then they will also stay with you in the hospital.
Anti-rejection medications
These medicines lower your body’s immune response. They will be started shortly before or after the transplant surgery and will continue for life. Without this therapy, your immune system will treat your new organ as a foreign body and the immunity cells in your body will start attacking it. It is vital to understand the timing, use and side-effects of these medicines. Your body’s immune system will weaken and so you will be informed about possible infections and how to keep away from catching them.
You will be prescribed other medications like antibiotics, to protect you from infections and anti-inflammatory medicines to reduce any signs of swelling and pain.
Most transplant organs start working effectively right after surgery while others may take a few weeks. Therefore, dialysis will be prescribed during this time.
Risks and complications of kidney transplant surgery
Short Term Complications
Besides a few general complications, such as pain, numbness or tingling in the thigh, a few other complications that may occur include:
- Infection
Minor infections like cold and flu may occur, which are treated using antibiotics. Serious infections, for example, urinary tract infections, Pneumonia and viral infections (CMV), may require hospital treatment. - Formation of Blood Clots
After surgery, the arteries connected to the donated kidney may develop clots at the site. You will be given blood-thinning medications to prevent this. If the blood supply to the organ is completely blocked, your doctor will advise you for its removal. - Arterial Stenosis
Arterial stenosis is the narrowing of the artery connected to the donated kidney, which can occur in some cases causing high blood pressure and may harm the organ. - Blockage of the Ureter
The tube carrying urine can be clogged with material like small clots or injured tissue during or after surgery. This is treated by placing a ‘Catheter’ (a narrow tube inserted to promote drainage) to clear off such clogging materials. - Acute rejection
The immune system recognises the donated kidney as a foreign tissue in the first year after surgery. If suspected, your doctor will run blood tests to confirm the diagnosis and your immunosuppressive or anti-rejection medicines will be changed.
Long Term Complications
Side effects of Immunosuppressive medicines:
These include:
- Risk of infection
- Higher risk of diabetes
- High blood pressure
- Diarrhoea and abdominal pain
- Hair loss
- Weight gain
- Gum swelling
- Easy bleeding
- Mood swings
- Cancer (rarely)
Finding the right dose of these medicines will take a few months depending on your body’s immunity.
Things to take care of while recovering
Quitting smoking and alcohol
People are encouraged to quit smoking and alcohol consumption before the transplant surgery to reduce after-surgery complications and organ rejection.
Diet
A healthy diet after transplant reduces food-related complications after surgery and maintains a healthy body weight, which further reduces the risk of heart disease, obesity and diabetes. You must follow the diet plan provided to you by your dietician and make frequent appointments to reassure that you are following it.
Exercise and Weight Loss
Your doctor will advise you to slowly increase your physical activity to walking, doing lighter exercises or physiotherapy. This will improve the functioning of your kidney graft, body weight, heart and overall quality of life.
You are also advised not to take medications without consulting your doctor (not even over the counter pain-killers).
Outcome of kidney transplant surgery
The success of this procedure depends on various factors like age, sex, health, body weight previous history of heart, liver or kidney diseases. Postoperative complications occur only in 15-17% of cases.
According to a report by Organ Procurement and Transplantation Network’ the survival of graft after one year of transplant surgery, especially in the Asian ethnicity was 95% with 97%.
Follow-up and support
After the surgery, you will be required to visit your doctor 2-3 times a week which will be reduced over time if there are no complications (like once every 3 to 6 months). Follow up is done to ensure the donated kidney is functioning properly, healing is taking at a normal pace, you are recovering as expected and there are no complications.
Seeking support
The process from diagnosis to successful operation and life after it can be challenging physically, socially, emotionally, and mentally. Finding the donor, taking multiple medical tests and financial burden of the treatment can be exhausting for both you and your caretakers. Depression, anxiety, frustration or sense of indecisiveness and worthlessness can be common after surgery.
You will need rehabilitation support like timely advice from your medical team, increasing your knowledge about your treatment, lifestyle, and diet with the help of your doctor, nurse, dietician, social workers, and so on. It is important for you to express your inner feelings during this time to your dear ones or friends and if needed, a certified psychologist. Seek help and do not isolate yourself emotionally during this period.
Surgery Cost In Your City
References
- National Health Services. Kidney Transplant: Overview. NHS-UK. Health A to Z. 2018 Aug 20.
- World Health Organisation. Human organ transplantation. WHO Newsletter. Health topics.
- Indian Society of Organ Transplantation. Statistics for Kidney. Indian Transplant Registry. Accessed on 2019 Jun 6.
- Jha, V. End-stage renal care in developing countries: the India experience. 2004 May 26. Renal Failure. 26: 201–208. PMID: 15354966
- Modi GK, Jha V. The incidence of end-stage renal disease in India: a population-based study.. 2006 Oct 25. Official Journal of the International Society of Nephrology. Kidney International. PMID: 17063176
- Kumar A, Singh NP. Kidney transplantation in India: Challenges and future recommendation. 2016 Jan 25. MAMC Journal of Medical Sciences; 2:12-7
- Khanna U. (2009). The economics of dialysis in India. 2009 Jan. Indian journal of nephrology. 19(1), 1–4. PMID: 20352002
- White SL, Chadban SJ, Jan S, Chapman JR, Cass A. How can we achieve global equity in provision of renal replacement therapy?. 2008 Mar. Bulletin of The World Health Organisation; 86(3):229-37. PubMed PMID: 18368211
- Garcia GG, Harden P, Chapman J. Global role of kidney transplantation.Hong Kong Journal of Nephrology. Volume 14, Issue 1, 2012, Pages 1-6, ISSN 1561-5413
- Moeller S, Gioberge S, Brown G. ESRD patients in 2001: global overview of patients, treatment modalities and development trends. 2002 Dec 1. Nephrology Dialysis Transplantation, Volume 17, Issue 12, Pages 2071–2076.
- National Organ and Tissue Transplant Organisation. Selection and Preparation of Kidney Transplant Recipient. Guidelines.
- Mehra NK, Chopra GS. Importance Of Donor Selection In Renal Transplantation. 1994 Jul. Medical journal Armed Forces India, 50(3), 205–210.
- National Organ and Tissue Transplant Organisation. Guidelines for the Management of Brain Dead Organ Donor in the Operation Theater (OT). Guidelines.
- Kiberd, B. A., AlBugami, M. M., Panek, R., & Tennankore, K. Contraindications to kidney transplantation: uneven grounds?. (2015). Transplantation research, 4, 2. PMID: 26203355
- Oxford Dictionaries. Graft: Definition. Lexico. British and World English.
- National Cancer Institute. [ink]. NCI Dictionary of Cancer Terms. Dictionaries.
- National Health Services. Having an operation (surgery): Before surgery. NHS-UK. Health A to Z. 2018 Feb 7.
- National Organ and Tissue Transplant Organisation. Guidelines For Kidney Transplantation – Living Donor Criteria. Guidelines.
- National Health Services. Having an operation (surgery): On the day. NHS Health A to Z. 2018 Feb 7.
- Kroner KT, Budgeon C, Colopy SA. Update on Surgical Principles and Equipment. 2016 Jan. The veterinary clinics of North America. Exotic animal practice. 19(1), 13–32. PMID: 26611922
- National Health Services. Kidney transplant: What happens . NHS-UK. Health A to Z. 2018 Aug 20.
- Lawrence L, Tran T, Mayo NE. What does it really mean to “recover” from an operation?. 2014. Surgery. Volume 155, Issue 2, 211 - 216.
- National Institute for Health and Care Excellence. Immunosuppressive therapy for kidney transplant in adults: The Technologies. 2017 Oct 11. NICE Guidance. Technology appraisal guidance [TA481].
- Reyna-Sepúlveda F, Ponce-Escobedo A, Guevara-Charles A, Escobedo-Villarreal M, Pérez-Rodríguez E, Muñoz-Maldonado G, Hernández-Guedea M. Outcomes and Surgical Complications in Kidney Transplantation. 2017 May 1. International Journal of Organ Transplantation Medicine. 8(2), 78–84. PMID: 28828167
- National Health Services. Kidney transplant: Risks . NHS-UK Health A to Z. 2018 Aug 20.
- Baker R, Mark PB, Patel RK, Stevens KK, Palmer N. Renal association clinical practice guideline in post-operative care in the kidney transplant recipient. 2017 Jun 2. BMC Nephrology. BMC series – open, inclusive and trusted. 18:174.
- Bertram L. Kasiske, Dagmar Klinger Jasn. Cigarette Smoking in Renal Transplant Recipients. April 2000. Journal of the AMerican Society of Nephrology. 11 (4) 753-759.
- Aref A, Sharma A, Halawa A. Smoking in Renal Transplantation; Facts Beyond Myth.. 2017 Apr 24. World Journal of Transplantation; 7(2):129-133. PubMed PMID: 28507915
- Nolte Fong JV, Moore LW. Nutrition Trends in Kidney Transplant Recipients: the Importance of Dietary Monitoring and Need for Evidence-Based Recommendations. 2018 Oct 31. Frontiers Medicine (Lausanne);5:302. PubMed PMID: 30430111.
- Romano G, Lorenzon E, Montanaro D. Effects of exercise in renal transplant recipients. 2012 Aug 24. World Journal of Transplantation; 2(4):46-50. PubMed PMID: 24175196.
- Gueye AS, Chelamcharla M, Baird BC, Nguyen C, Tang H, Barenbaum AL, Koford JK, Shihab F, Goldfarb-Rumyantzev AS. The association between recipient alcohol dependency and long-term graft and recipient survival. 2007 Mar. Nephrology Dialysis Transplantation. Volume 22, Issue 3, Pages 891–898
- Reyna-Sepúlveda F, Ponce-Escobedo A, Guevara-Charles A, Escobedo-Villarreal M, Pérez-Rodríguez E, Muñoz-Maldonado G, Hernández-Guedea M. Outcomes and Surgical Complications in Kidney Transplantation. Epub 2017 May 1. Int J Organ Transplant Med. 2017;8(2):78-84. PubMed PMID: 28828167
- Gupta G, Unruh ML, Nolin TD, Hasley PB. Primary Care of the Renal Transplant Patient. Epub 2010 Apr 27. Journal of General Internal Medicine. 25(7):731-40. PubMed PMID: 20422302
- Pawar AA, Rathod J, Chaudhury S, Saxena SK, Saldanha D, Ryali VS, Srivastava K. Cognitive and emotional effects of renal transplantation. 2006. Indian Journal of Psychiatry. 48(1), 21–26.