Summary
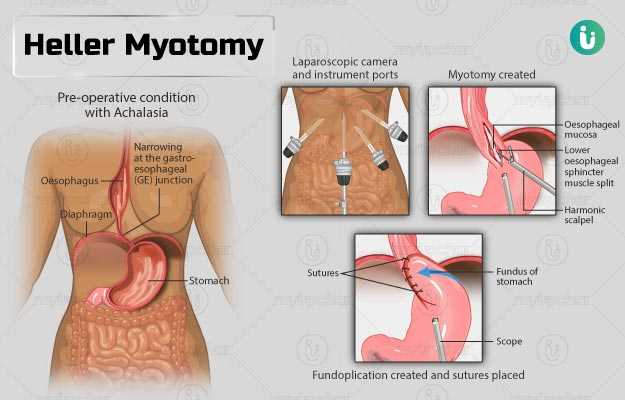
Heller myotomy is performed to treat achalasia, a condition that causes difficulty in swallowing solid food and liquids. Achlasia is caused due to stiffening of the lower oesophageal sphincter, a ring of muscle fibre present at the junction of the oesophagus (food pipe) and the stomach. This sphincter prevents the backflow of stomach contents into the oesophagus. However, if this sphincter becomes stiff, it does not allow the entry of food from the oesophagus into the stomach.
This surgery is usually performed as a laparoscopic procedure, which requires multiple tiny cuts in the abdomen. If the laparoscopic approach cannot treat the condition, the surgeon performs an open surgery, which requires a larger incision near the midline of the abdomen. You will be required to stay at the hospital for one to seven days, depending on whether the surgery was open or laparoscopic surgery. You will be able to continue with your normal activities after three to four weeks of the procedure.
- What is Heller myotomy?
- Why is Heller myotomy recommended?
- Who can and cannot get Heller myotomy?
- What preparations are needed before Heller myotomy?
- How is Heller myotomy done?
- How to care for yourself after Heller myotomy?
- What are the possible complications/risks of Heller myotomy?
- When to follow up with your doctor after a Heller myotomy?
What is Heller myotomy?
Heller myotomy is a surgical procedure that is done for the treatment of a condition called achalasia.
Achalasia is a disorder of the oesophagus (food pipe) that causes difficulty in swallowing. The oesophagus is a muscular tube that carries liquid and food from the throat to the stomach. The lower end of the oesophagus that connects to the stomach is guarded by a ring-like muscle called the sphincter. This sphincter prevents the backflow of food from the stomach to the oesophagus. Normally, when you swallow food, this sphincter relaxes to allow the food to pass into the stomach. However, in individuals with achalasia, this sphincter does not open properly. Hence, the food gets stuck in the oesophagus, and often comes back to the mouth. This difficulty in swallowing is usually resolved after taking small sips of water.
The exact reason for the condition is not known; however, damage to the nerve cells in the sphincter muscles can be a reason.
Heller myotomy helps to improve swallowing in individuals with achalasia by cutting the muscle fibres of the lower oesophageal sphincter.
The name Heller myotomy comes from the fact that it was first performed by Ernest Heller in the year 1913, while a myotomy is any procedure which involves cutting of a muscle.
Why is Heller myotomy recommended?
Your surgeon will recommend this surgery if you show the following symptoms of achalasia:
- Difficulty swallowing liquid and food
- Chest pain
- Drooling of saliva or vomiting
- Frequent chest infections
- Significant weight loss over a period of time
- Heartburn
- Coughing and choking
Although not every individual will show symptoms of achalasia, symptoms such as swallowing difficulty can develop over a period of about two years. If left untreated, achalasia can develop into oesophageal cancer.
The following tests may be performed to confirm achalasia:
- Oesophageal manometry study: A test performed by inserting a small tube through your nose down the throat to measure the pressure in the lower oesophageal sphincter and oesophagus.
- Barium swallow test: A special type of X-ray that allows the doctor to observe the oesophagus when you swallow.
- Diagnostic gastroscopy: A test performed by inserting a long tube through the mouth to look at your oesophagus.
Who can and cannot get Heller myotomy?
A doctor may not recommend this surgery in individuals with the following conditions as they can increase the risks of surgery:
- Lung diseases, heart diseases, or kidney diseases
- Pregnancy
- Smoking habit Read more: Harmful effects of smoking on health
What preparations are needed before Heller myotomy?
You may need the following preparations before the surgery:
- The surgeon may discuss the following with you before the surgery:
- Avoid eating or drinking anything from the midnight before the surgery to prevent the following under the effect of anaesthesia:
- Vomiting
- The entry of food into the lungs
- While going to the hospital for the surgery, take care of the following:
- Wear loose, comfortable clothes
- Do not wear any jewellery, makeup, nail polish or dentures
- Ask a responsible adult to drive you home after the surgery
How is Heller myotomy done?
After arriving at the hospital, the hospital staff will ask you to change into a hospital gown, and you will be taken to the operating room. Your blood pressure, heart rate, and oxygen levels will be continuously monitored during the procedure. An intravenous (IV) line will be placed in your hand. The types of anaesthesia that may be used during the surgery include:
- General anaesthesia: Makes you fall asleep during the procedure. General anaesthesia is usually used during the procedure.
- Regional anaesthesia: Numbs a large part of the body, but keeps you awake. This anaesthesia may be used alone or in combination with general anaesthesia.
- Local anaesthesia: Numbs a small part of the body and keeps you awake. This anaesthesia may be injected around the surgical site to provide pain relief.
Heller myotomy can be performed by two methods, namely open and laparoscopic. Laparoscopic is usually the preferred method since it is associated with minimum pain post-surgery and faster recovery. However, if the procedure cannot be completed by the laparoscopic approach, open surgery will be performed. Open surgery results in a large scar and requires an extended stay in the hospital.
The laparoscopic procedure involves the use of a long thin camera and other tools inserted through tiny cuts on the body. The camera allows the surgeon to view your internal structures on a television. The surgery usually involves the following steps:
- An anesthesiologist will administer anaesthesia to you.
- The surgeon will make about five small incisions on your abdomen, above your belly button.
- He/she will push carbon dioxide gas into your abdomen to inflate it. This will give the surgeon more area to use the surgical instruments and view your organs.
- After accessing the oesophagus, the surgeon will make small cuts in the stiffened sphincter muscle.
- As there is a risk of stomach acid going back up into the oesophagus (acid reflux) after the surgery, the surgeon will perform a fundoplication after this procedure. This includes wrapping the top end of the stomach around the oesophagus like a wrap and fixing it in place with sutures such that it functions like a valve and helps prevent acid reflux.
- If the laparoscopic approach is not viable, open surgery is done that requires a relatively larger vertical incision at or near the midline of the abdomen.
The laparoscopic procedure requires one to two days of hospital stay, while the open procedure requires you to stay in the hospital for about a week. After the surgery, you will be transferred to the recovery room and can expect the following:
- Your vital signs will be closely monitored.
- The medical staff may administer fluids through a drip.
- The doctor may give you some medicines to provide relief from the pain.
- A special type of X-ray called barium oesophagram may be performed to examine your oesophagus.
- You may be given fluids to drink after you wake up from the surgery. If you are comfortable with drinking liquids, you can start with soft foods from the next day.
How to care for yourself after Heller myotomy?
The surgeon will recommend the following care at home after a Heller myotomy:
- It may not be easy to swallow food during the initial days after the surgery. Hence, you should chew the food well and eat a small amount of food at a time.
- Take soft food for two weeks after the surgery. Avoid eating bread for six to eight weeks. You will need to permanently exclude fizzy drinks from your diet.
- You may still experience some acid reflux after fundoplication surgery. The surgeon may prescribe some medicines for the same.
- Your oesophagus may take about six to eight months to heal completely. However, you will be able to get back to your daily routine in about six to eight weeks.
- You will be able to resume driving after three to four days (after a laparoscopic procedure) or about 10 days (after open surgery).
Heller myotomy helps to remove the obstruction in the oesophagus and improves swallowing.
When to see the doctor?
Contact the surgeon if you experience any of the following:
- Increased pain or discomfort
- Nausea and vomiting
- Difficulty emptying the bladder
- Swelling, redness, or drainage at the site
- Fever above 101°F
- Reopening of the wound
- Diarrhoea
- Constipation
What are the possible complications/risks of Heller myotomy?
The complications associated with the surgery include:
- Damage to the inner wall of the oesophagus
- Wound infection
- Damage to the spleen or other abdominal organs
- Formation of blood clots in the leg that can spread to the lungs
- Scarring at the surgery site
- Adverse reaction to surgical materials
- Complications of general anaesthesia such as:
- Lung infection
- Confusion
- Drug allergy
- Heart attack
- Need for another surgery to remove the scar tissue or problems in other muscle fibres
When to follow up with your doctor after a Heller myotomy?
You will have a follow-up visit in about six weeks after the surgery and then at three months for a post-operative assessment.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Find Gastroenterologist in cities
- Gastroenterologist in Gurgaon
- Gastroenterologist in Bangalore
- Gastroenterologist in Chennai
- Gastroenterologist in Jaipur
- Gastroenterologist in Ahmedabad
- Gastroenterologist in Noida
- Gastroenterologist in Mysore
- Gastroenterologist in Visakhapatnam
- Gastroenterologist in Hyderabad
- Gastroenterologist in Pune
Surgery Cost In Your City
Doctors for Heller myotomy

Dr. Rishabh Gupta
Gastroenterology
6 Years of Experience

Dr. Paramjeet Singh.
Gastroenterology
10 Years of Experience

Dr. Nikhil Bhangale
Gastroenterology
10 Years of Experience

Dr Jagdish Singh
Gastroenterology
12 Years of Experience
References
- Cambridge University Hospitals [internet]: NHS Foundation Trust. National Health Service. U.K.; Patient information and consent to laparoscopic heller’s myotomy for achalasia
- National Health Service [internet]. UK; Achalasia
- Smith G, Goldman J. General Anesthesia for Surgeons. [Updated 2020 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- East Kent Hospitals University [internet]: NHS Foundation Trust. National Health Service. U.K.; Achalasia
- Hernandez A, Sherwood ER. Anesthesiology principles, pain management, and conscious sedation. In: Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston Textbook of Surgery. 20th ed. Philadelphia, PA: Elsevier; 2017:chap 14.
- Cohen NH. Perioperative management. In: Miller RD, ed. Miller's Anesthesia. 8th ed. Philadelphia, PA: Elsevier Saunders; 2015:chap 3.
- Stanford Health Care [internet]. Stanford Medicine. Stanford Medical Center. Stanford University. US; General Surgery Preparation
- American Society of Anesthesiologists [Internet]. Washington D.C. US; Types of Anesthesia
- Memorial Hermann Foundation [Internet]. US; Laparoscopic Heller Myotomy
- Abir F, Modlin I, Kidd M, Bell R. Surgical treatment of achalasia: current status and controversies. Dig Surg. 2004. 21 (3):165-76. PMID: 15218230.
- von Rahden BHA. [Current Treatment of Achalasia 2019]. Zentralbl Chir. 2019 Apr. 144 (2):163-170. PMID: 30978762.
- Patti MG, Fisichella PM. Controversies in management of achalasia. J Gastrointest Surg. 2014 Sep. 18 (9):1705-9. PMID: 24972973.
- Tapias LF, Morse CR, Mathisen DJ, Gaissert HA, Wright CD, Allan JS, et al. Surgical Management of Esophageal Epiphrenic Diverticula: A Transthoracic Approach Over Four Decades. Ann Thorac Surg. 2017 Oct. 104 (4):1123-1130. PMID: 28847539.
- Morino M, Famiglietti F, Giaccone C, Rebecchi F. Robot-assisted Heller myotomy for achalasia: technique and results. Ann Ital Chir. 2013 Sep-Oct. 84 (5):520-3. PMID: 24140614.
- Misra L, Fukami N, Nikolic K, Trentman TL. Peroral endoscopic myotomy: procedural complications and pain management for the perioperative clinician. Med Devices (Auckl). 2017 Feb 23. 10:53-59. PMID: 28260955.
- Fischer JE. Mastery of Surgery. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2007
- Gouda BP, Nelson T, Bhoyrul S. Revisional surgery after heller myotomy for treatment of achalasia: a comparative analysis focusing on operative approach. Indian J Surg. 2012 Aug. 74 (4):309-13. PMID: 23904720.
- Allaix ME, Patti MG. Heller myotomy for achalasia. From the open to the laparoscopic approach. World J Surg. 2015 Jul. 39 (7):1603-7. PMID: 25526923.
- Moonen A, Boeckxstaens G. Current diagnosis and management of achalasia. J Clin Gastroenterol. 2014 Jul. 48 (6):484-90. PMID: 24926623.
- Katilius M, Velanovich V. Heller myotomy for achalasia: quality of life comparison of laparoscopic and open approaches. JSLS. 2001 Jul-Sep. 5 (3):227-31. PMID: 11548827.
- Mandovra P, Kalikar V, Patel A, Patankar RV. The laparoscopic approach for epiphrenic diverticula with achalasia. Ann R Coll Surg Engl. 2019 Apr. 101 (4):256-260. PMID: 30773891.
- Patel K, Abbassi-Ghadi N, Markar S, Kumar S, Jethwa P, Zaninotto G. Peroral endoscopic myotomy for the treatment of esophageal achalasia: systematic review and pooled analysis. Dis Esophagus. 2016;29(7):807-819. PMID: 26175119.
- Vaezi MF, Richter JE. Current therapies for achalasia: comparison and efficacy. J Clin Gastroenterol. 1998;27(1):21-35. PMID: 9706766.
- Shiino Y, Filipi CJ, Awad ZT, Tomonaga T, Marsh RE. Surgery for achalasia: 1998. J Gastrointest Surg. 1999;3(5):447-455. PMID: 10482699.
- Andreollo NA, Earlam RJ. Heller's myotomy for achalasia: is an added anti-reflux procedure necessary?. Br J Surg. 1987;74(9):765-769. PMID: 3311282.
- Veenstra BR, Goldberg RF, Bowers SP, Thomas M, Hinder RA, Smith CD. Revisional surgery after failed esophagogastric myotomy for achalasia: successful esophageal preservation. Surg Endosc. 2016;30(5):1754-1761. PMID: 26275539.
- UCSF Department of Surgery [internet]. University of California San Francisco. California. U.S.A.; Heller Myotomy
- Michigan Medicine: University of Michigan [internet]. US; Instructions Following Abdominal Surgery
- Northwestern Medicine [internet]. Northwestern Memorial HealthCare. Northwestern University. Illinois. U.S.; Heller Myotomy