Summary
The surgical removal of the tongue is called glossectomy. It is recommended to individuals who have been diagnosed with tongue cancer. Glossectomy is of the following types: partial, hemi, subtotal and total. This operation may give rise to speech and swallowing problems, for which speech and swallow therapy may be needed.
- What is glossectomy?
- Why is glossectomy recommended?
- Who can and cannot get glossectomy?
- What preparations are needed before glossectomy?
- How is glossectomy done?
- How to care for yourself after glossectomy?
- What are the possible complications/risks of glossectomy?
- When to follow up with your doctor after a glossectomy?
What is glossectomy?
Glossectomy is a surgical procedure to remove a part of or the entire tongue primarily to treat cancers of the tongue, mouth and throat.
Your tongue is made of two parts – the oral tongue (front part) and the base of the tongue (part of the throat). The functions of the tongue include tasting, swallowing, breathing, licking and speaking.
How much of the tongue will be removed during glossectomy is decided based on the size and location of the tumour. If the tumour is small, the hole left after removal of the tumour will be stitched or left to close naturally; whereas, if the tumour is large, the hole may be filled with a piece of skin or muscle known as a flap. Once the tumour is removed, it will be sent for microscopic examination, and depending on the results, you may need additional treatment. Some normal, healthy tissues around the tumour will also be removed to ensure that no cancer cells are left behind.
The tongue is a common site for oral cancer and, when detected early, it is highly curable. When cancer forms in the front two-third part of the tongue, it is classified as a type of oral cavity cancer, known as oral tongue cancer. Cancer that develops in the remaining third of the tongue is classified as throat cancer and called tongue base cancer. The choice of treatment for tongue cancer is usually surgery with or without other therapies, such as radiation or chemotherapy.
Why is glossectomy recommended?
Glossectomy is generally recommended for tongue cancer, which is a type of head and neck cancer with symptoms as follows:
- A white or red patch on the tongue, an ulcer or lump on the tongue, or a feeling of numbness in the mouth that does not go away
- A sore throat that persists
- Pain while swallowing
- Unexplained bleeding from the tongue
- Ear pain (rarely)
Glossectomy may also be done for correcting an unusually large tongue (macroglossia), which can cause difficulties with speech, chewing, swallowing and breathing. Macroglossia is seen in conditions such as Beckwith-Wiedemann syndrome.
Individuals with the following characteristics are at a higher risk of developing tongue cancer and may need a glossectomy:
- Use tobacco
- Spend more time in the sun, especially exposing the lips to more sunlight
- Have excessive alcohol consumption
- Have exposure to human papillomavirus
- Have a weak immune system due to other health conditions
- Smoke (smokers are five times more prone to tongue cancer than non-smokers) Read more: Effect of smoking on oral health
- African-American men as they have a higher risk than Caucasians
Who can and cannot get glossectomy?
Glossectomy is contraindicated in the following cases:
- Individuals who are medically unfit, malnourished, unable to give informed consent, unable to overcome speech and swallowing challenges, have poor social support and are unable to finish adjuvant therapy.
- Individuals with tumours that do not have clearly defined margins or have distant metastases (cancer cells that break away from the original site and spreads to other organs).
- Some contraindications for partial glossectomy are – cancer that has invaded into the nearby structures or has crossed the midline of the tongue as partial glossectomy requires that one lingual artery and hypoglossal nerve (the artery and nerve that supply to the tongue) be preserved.
What preparations are needed before glossectomy?
The decision to perform a glossectomy generally depends on the stage of cancer, where it is located on the tongue and the overall health of the individual. However, before going for the treatment, it is important to find out the stage of cancer to decide the type of glossectomy to be done. Your healthcare provider will check your medical history and presence of risk factors such as tobacco use or alcohol consumption. He/she may ask you certain questions, such as the timing when the symptoms of cancer developed and if the symptoms have changed in appearance (or size). Imaging tests or a biopsy may be done to assess the cancer and its spread.
Tests done for diagnosis are as follows:
- Biopsy: A small sample of tissues will be removed from the affected area. A biopsy can be done in three ways:
- Fine needle aspiration biopsy: A thin needle will be inserted into the tumour mass, and a sample will be withdrawn by suction into a syringe.
- Incisional biopsy: A sample will be taken using a surgical knife (scalpel).
- Punch biopsy: With the help of a small circular blade, a round area of affected tissue will be removed.
- X-ray of the mouth and throat
- Computed tomography (CT) scan
- Positron emission tomography (PET) scan
The five stages of cancer are:
- Stage 0: It is also referred to as carcinoma in situ and is just the beginning stage.
- Stage I: It describes an early stage where the tumour is not more than 2 cm, and cancer has not spread to the lymph nodes.
- Stage II: In this stage, the tumour is larger than 2 cm but not more than 4 cm and has not yet spread to the lymph nodes.
- Stage III: Here, the tumour size is either larger than 4 cm or it has spread to lymph nodes in the neck.
- Stage IV: This stage is the most advanced stage with cancer of any size that has spread to the nearby tissues, lymph nodes and distant parts of the body.
Cancers in stages III and IV are most likely to recur than early-stage cancers. The most common treatments for tongue cancer are surgery, chemotherapy and radiation therapy.
The following are some other preparations that are needed before a glossectomy:
- You may require an electrocardiogram.
- You may need to have blood tests such as complete blood count, blood clotting time test and liver function tests.
- Heart and lung function tests may also be needed to ensure you are healthy for the surgery. Read more: What is stress test
- A nutritional assessment will be done to check your weight and food intake.
- You must take a full dental check-up and receive dental care as a part of the treatment plan.
- You should stop smoking as it slows down the healing process, increases the risk of side effects of surgery and also increases the risk of recurrence of cancer.
- You should not eat or drink anything except necessary medicines any time after midnight before the operation.
- Inform the doctor if you have fever, cough or any other signs of infection.
How is glossectomy done?
The hospital procedure on the day of surgery will be as follows:
- You must arrive at the hospital a few hours before the scheduled time of operation.
- Make sure to brush your teeth and tongue in the morning before the operation and also gargle with a mouthwash after brushing.
- You will be asked to sign a consent form to give permission to the doctor to perform the surgery.
- If you have to take medicine, take it with a small sip of water.
- You will have to scrub your neck and chest with a special brush to clean the skin of germs which can cause infection.
- The doctor will communicate to you if you need to shave the area.
- An intravenous (IV) line will be introduced into a vein in your arm to provide you with fluids and medications as and when required.
- The surgery area will be marked with a special pen.
- You will be given general anaesthesia, which will put you to sleep.
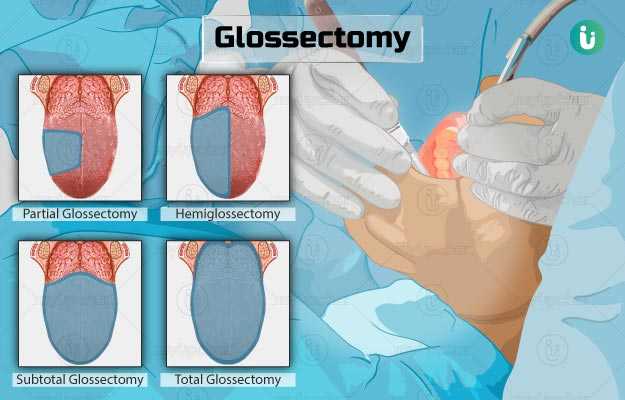
The types of glossectomy are as follows:
- Partial glossectomy: This procedure includes the removal of a part (the affected part) of the tongue. After removing the part of the tongue, the wound will be closed either with stitches or allowed to self-heal. If a large part is cut, a skin graft or reconstruction might be required to close the wound. Usually, speech and swallowing problems are not likely after this procedure.
- Hemiglossectomy: This procedure includes removal of just one side of the tongue, leaving the other side intact.
- Subtotal glossectomy: Subtotal glossectomy is used to treat larger tumours of the tongue. During this procedure, the doctor will remove a large part of your tongue, and perform reconstruction surgery to repair the wound so that you can swallow and speak as well.
- Total glossectomy: This procedure includes removal of the whole tongue. A laryngectomy (removal of the larynx – the voice box) may be performed along with a total glossectomy if the cancer has spread to the larynx. This surgery makes eating and speaking difficult. For laryngectomy, the surgeon will create an opening (stoma) in your neck (tracheostomy) and attach the end of the windpipe to it. The tracheostomy could be permanent, and speaking normally may not be possible.
A partial or hemi glossectomy is chosen to remove small tumours from the tongue. The remaining area will be stitched so that there is no hole. At times, a small piece of skin may be used to fill in the hole. A total glossectomy requires major reconstructive surgery.
After the surgery is completed, the following steps will take place:
- You will be moved to a recovery room and will be closely monitored by a nurse until you are fully awake.
- When you wake up, you may have a tube in your neck for breathing, more tubes in your body for draining fluid and feeding.
- The IV line will provide fluids until you feel better and can swallow. Your medicines will also be administered through the IV line.
- A nurse will clean your mouth every four hours using a large syringe filled with a solution.
- If you are allowed to go home the same day, you will have to learn the procedure for rinsing your mouth as it is important to do this every time after you eat.
- Based on the extent of the surgery and the sensation and movement of the remaining tongue, you may need to meet a speech therapist to learn to speak and swallow after the surgery.
- On average, the hospital stay is for one to two days, but a reconstructive surgery using a flap may increase the stay up to two weeks.
How to care for yourself after glossectomy?
After glossectomy, the following care needs to be taken:
- Wound care: Your doctor will prescribe you a mouthwash to keep your mouth clean and prevent any wound infection. You must ensure that food and debris do not get trapped in your mouth. Make sure to rinse your mouth with water every time after you eat/drink anything. You will be prescribed a pain medicine in liquid form if needed so that you can easily swallow it.
- Diet care: You may begin taking fluids such as juice, milk, milkshakes, puddings, ice cream and strained soups after the surgery. Your doctor will inform you about when to start soft foods. Sometimes, eating and drinking may be a problem after a glossectomy. In such cases, a small feeding tube may be placed in your nose during the surgery for nutrition. The feeding tube will be taken off once you are able to eat/drink by mouth. A swallow therapist will guide you with this transition.
- Activity: You will be asked to move around after the surgery to prevent breathing and circulation problems. It will also help you build strength and recover quickly. You shall be able to sit at the bedside within two to six hours after surgery. Your doctor will ask you to do deep breathing and exercises to improve circulation. You can resume your regular activities slowly over the next few weeks. However, avoid indulging in strenuous exercises for the first week. Do not lift anything over 25 lb for the first two weeks. You must not drive until your strength and speed of movement return to normal.
- Speech care: Mostly, people can speak fairly clear after the surgery. However, if your speech is affected by the surgery, a speech-language pathologist will help you to assess your ability to speak and will tell you how to improve your communication. You might sound different depending on how much of your tongue was removed. If the entire tongue has been removed, you might not be able to talk at all. You will need a speech therapist to help you with communication.
When to See the Doctor?
You must immediately visit your doctor if you have the following symptoms:
- Increased pain in tongue
- A fever of more than 102°F
- Change in the way your mouth tastes or breath smells
- Pus-like drainage from the tongue
- A change in the colour of tissue of the tongue (white, black or grey)
- Difficulty in opening the jaw
- Changes in vision, hearing or taste
- Difficulty in chewing, speaking or swallowing
- New lump or swelling in the neck or mouth
What are the possible complications/risks of glossectomy?
Glossectomy may have the following complications:
- Haematoma (blood accumulation that may go away on its own or require surgery)
- Infection
- Salivary fistula formation (a hole that causes saliva to leak from the mouth into the neck)
- Airway blockages (blocking of the airways, which leads to difficulty in breathing)
- Aspiration (food or fluid that is not swallowed properly enters into the lungs instead of the stomach)
- Pneumonia
- Poor speech or difficulty speaking (dysarthria) or loss of speech
- Difficulty in swallowing (dysphagia)
- Flap failure (due to issues with blood supply to the flap used for reconstruction of the tongue)
- Bleeding from the tongue
- Weight loss
When to follow up with your doctor after a glossectomy?
Follow-up visits are generally scheduled every one to three months in the first year, every two to six months for the second year, every four to eight months for the third to fifth year and every 12 months from the sixth year onward.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- Oncolink [Internet]. Philadelphia: Trustees of the University of Pennsylvania; c2018. Surgical Procedures: Glossectomy
- Imperial College Healthcare NHS Trust [internet]. National Health Service. UK; Imperial College Healthcare
- UAB Medicine [Internet]. UAB Health System. Alabama. US; Partial/ Total Glossectomy
- Cancer Research UK [Internet]. London. UK; What is tongue cancer?
- Victor. S, et al. Partial glossectomy in a patient carrier of Beckwith–Wiedemann syndrome: Presentation of a case. Revista Española de Cirugía Oral y Maxilofacial (English Edition). October–December 2015; 37(4): Pages 202-206
- MOFFITT Cancer Center [Internet]. Florida. US; What Are the First Signs of Tongue Cancer?
- Cedars Sinai [Internet]: Cedars Sinai Medical Center. Los Angeles. US; Tongue Cancer
- Eugene N.M, Carl H.S. Operative Otolaryngology:Head and neck surgery. 3rd ed. Elseiver.
- Canadian Cancer Society [internet]. Toronto. Canada; Surgery for oral cancer
- St. Joseph's Healthcare Hamilton [Internet]. Ontario. Canada; Partial Glossectomy Surgery
- Thancguide [Internet]. Thyroid, Head and Neck Cancer Foundation. New York. US; Glossectomy
- UW Health: American Family Children's Hospital [Internet]. Madison (WI): University of Wisconsin Hospitals and Clinics Authority; Glossectomy