Summary
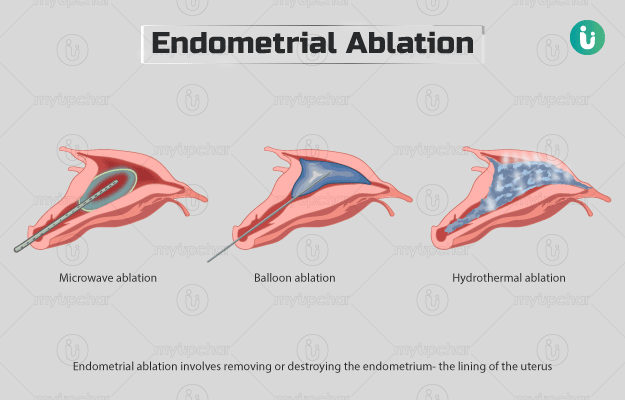
Endometrial ablation is a procedure that is done for the treatment of heavy periods. In this procedure, the surgeon removes the endometrium or the inner lining of the uterus using extremely cold temperature (cryoablation), electric current (electrocautery), or heated fluid (hydrothermal). The procedure does not need any cuts or incisions, instead, a hysteroscope or other instruments are inserted in through the vagina.
You will have to undergo a biopsy prior to the procedure. Also, fasting for at least eight hours is also necessary. On the day of the procedure, your doctor will suggest you to take sanitary napkins to the hospital as you will be bleeding for a while afterwards.
Women who undergo this procedure may not be able to get pregnant afterwards.
Initially, after the surgery, your periods will still be heavy. However, the flow will gradually reduce over the months. You must refrain from heavy lifting, strenuous activities, and sexual intercourse for a few weeks after this procedure. to allow proper healing of the operated area.