Summary
Discectomy involves the removal of a part of a degenerated or herniated (slipped or ruptured) intervertebral disc (the cushion-like disc between two vertebrae). This surgery is indicated - when all other treatments fail - in case of increasing neurological deficit and severe, persistent pain that radiates to other areas from the spine.
Discectomy is not indicated for severe disc degeneration that leads to the narrowing of the spinal canal; nerve compression; hardening of the longitudinal spinal ligaments, interspaces and discs; and slippage of vertebrae. For many individuals, this surgery relieves nerve pressure, and they can go back to their normal activities with improved symptoms of bladder and bowel control.
- What is discectomy?
- Why is discectomy recommended/done?
- Who can and cannot get a discectomy?
- What preparations are needed before discectomy?
- How is discectomy done?
- How to care for yourself after discectomy?
- What are the possible complications/risks of discectomy?
- When to follow up with your doctor after a discectomy?
What is discectomy?
Discectomy is a surgical procedure that involves the removal of a degenerated or herniated part of an intervertebral disc (a part of the spinal column).
The spinal column in humans is made up of vertebral bodies (vertebrae) extending from the base of the skull to the coccyx and is divided into cervical (neck area), thoracic (chest area), lumbar (abdominal area) and sacral regions (below the abdominal area). The vertebrae are separated from one another by cushion-like structures called intervertebral discs.
Intervertebral discs are cartilaginous structures composed of an outer structure (annulus fibrous), which is a tough yet flexible, dense collagenous ring that surrounds the inner structure (nucleus pulposus), and endplates that serve to hold the discs to the adjacent vertebrae. Overall, the separating discs lend support to the entire spine by acting as shock-absorbing cushions.
A herniated/degenerated disc occurs when the outer annulus fibrous tears or breaks down and the inner nucleus pulposus protrudes and presses against the nerves located in that region or exerts pressure on the spinal cord, resulting in pain and discomfort. This often occurs due to age-related degenerative process that causes the nucleus pulposus to become less hydrated and weak. Trauma or injury to the spine may be additional causative factors of disc herniation.
Disc herniation is most common in the lumbar region of the spine, followed by the cervical spine.
Why is discectomy recommended/done?
Discectomy is recommended for individuals with the following conditions:
- Radiculitis: Radiculitis refers to pain radiating from the knee down along the sides and back of the leg. Pain may sometimes be experienced on the frontal portion of the thigh or groin.
- Cauda equina syndrome: Cauda equina syndrome occurs when the cauda equina nerve bundle lying at the end of the spinal cord gets damaged. A person with this syndrome experiences leg pain with tingling, numbness and weakness, and loss of bladder or bowel control. Sensory abnormalities in the sex organs (genitalia), anal region, and perineum.
- Functional weakness: Weakness in muscles that are important for functioning such as muscles in the ankles and hips, numbness in certain parts of the lower body and loss of bowel or bladder control among other things, and progressive neurological deficit (increasing problems with nerve function in a certain area). Back pain that persists despite treatment and affects the quality of life,
- Sciatica: Pain along the distribution of the sciatic nerve with increased sensitivity to pain, which is not relieved with medicines. Paralysis caused due to sciatica.
- Persistent radiating pain that limits regular movements despite treatment.
Who can and cannot get a discectomy?
The first-line of treatment and pain management in disc herniation includes medications, physiotherapy and rest. Often, pain of the radiating kind will reduce or subside within six weeks. If there is no overall improvement, epidural steroid injections (injection of medicine in the region of the spinal nerves) may be administered to cope with the pain and discomfort. Individuals with persistent symptoms extending beyond six weeks and abnormalities on MRI scan are recommended for surgery.
There are no absolute contraindications to discectomy; however, there are some contraindications to certain methods used for a discectomy as follows
- An open discectomy is contraindicated in individuals with severe degenerative facet disease (degeneration of the facet joints in the spine), calcified disc herniation (calcification/hardening of the protruding disc) and spinal stenosis (narrowing of the spaces in the spine). This method is usually recommended for people with the following conditions:
- Spondylolisthesis (vertebral bone slips onto the bone below it)
- Severely degenerated discs
- Disc herniation between the L5-S1 vertebrae
- Disc herniation that occupies more than 30% of the spinal canal
- Extruded/sequestered disc herniation
- Previous surgery with scar tissue entrapment (nerve trapped/pinched due to scar tissue)
- Bone spur impingement on the nerve root (pinching of the nerve root due to bony growths)
- Calcification (hardening) of longitudinal ligaments, interspaces, and discs associated with higher degree of technical difficulty during surgery.
- The main and common contraindications to minimally invasive percutaneous, arthroscopic and endoscopic microdiscectomy are extruded/sequestered disc fragments (disc fragments that bulge out of the disc or are free from the disc).
- Laser discectomy is indicated for disc herniation that can be observed on radiological tests, if there is no relief after a minimum of six weeks of conservative therapy, and if the first part of the nerve is formed from a single disc. The contraindications for percutaneous laser discectomy include sequestered disc fragments, severe spinal stenosis, calcified posterior spinal ligament, scar tissue from the previous microsurgery, transannular extrusion, and severe spondylosis (wear and tear due to old age).
What preparations are needed before discectomy?
The preparations needed before surgery are as follows:
- You will be asked to undergo medical evaluation as per your doctor’s recommendation. Commonly, evaluations such as chest X-ray, blood tests and electrocardiogram, are performed.
- You will also be explained the details of your discectomy along with the side-effects and complications.
- You will need to sign a document providing consent to the procedure.
- Your doctor will ask you about your medical history and pre-existing medical conditions such as diabetes, heart problems or blood-related disorders.
- If you are pregnant or suspect you are pregnant, you should inform your doctor about it.
- Also, let your doctor know of all the medications and supplements you are consuming as some of those may need to be reduced or temporarily stopped for the surgery.
- You should stop consuming alcohol and smoking prior to the surgery as it may affect your recovery.
How is discectomy done?
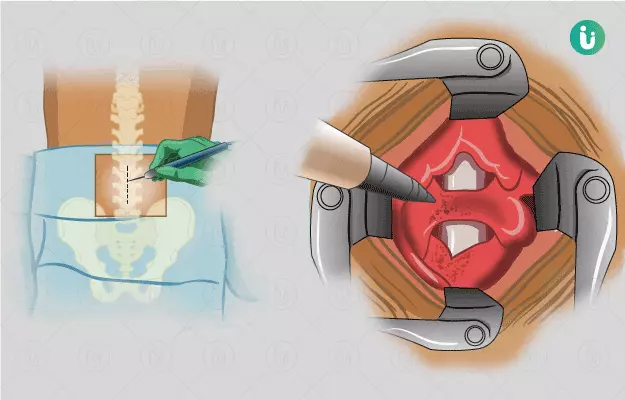
For discectomy surgery, you will be asked to lie on the operation table. Depending on the type of surgery, general or local anaesthesia will be given. Once you are asleep, the healthcare provider will roll you onto the stomach and support your chest and sides with pillows. The area of incision is cleaned and prepared.
For open discectomy, the following steps are further performed under general anaesthesia.
- A tube will be introduced in your throat to help you breathe.
- The surgeon will identify the area of surgery and cleanse it.
- Then, he/she will make a 3-5-cm long incision in that region, and the muscles in the area will be moved to one side for better accessibility.
- The surgeon may also remove some parts of the bone and ligament so that the disc and the nerve can be made visible. This procedure is known as laminotomy.
- Next, the part of the nucleus pulposus that has leaked out through the tear will be removed, and the annulus will be trimmed so that the disc is no longer pushing against the nerve.
For arthroscopic microdiscectomy, the following steps are performed under local anaesthesia:
- The surgeon will make an incision (1 cm) in the skin of the affected area to insert one or two ports (tubes).
- He/she will observe the nerves, adjacent structure and external part of annulus using an arthroscopic instrument attached with a camera.
- The surgeon will position one or two cannulas (hollow tubes) on the outer layer of the annulus by passing through the skin and muscle layers of the area.
- Next, he/she will insert two more tubes either on the same side or one on left and one on the right to make a path to the affected disc.
- With this surgery, the surgeon is able to see and remove herniated fragments even beyond the annulus and nucleus pulposus.
For minimally invasive percutaneous discectomy, the following steps are performed:
- The surgeon will make a small incision on one side of your back.
- He/she will use a series of larger dilators to create a tunnel to the vertebrae by separating the muscle.
- Next, the surgeon will make a small opening around your spinal nerve using a drill and perform a laminotomy.
- The surgeon will retract the protective sac of the spinal nerve root.
- He/she will use a surgical microscope to find the herniated disc. Once the ruptured part is removed, the nerve root will be decompressed.
For laser discectomy, the following steps are performed under local anaesthesia:
- Your doctor will make a small cut on your back and identify the disc that is to be operated on.
- He/she will insert a thin, hollow needle inside this disc.
- With the help of radiological methods such as fluoroscopy and magnetic resonance imaging (MRI), the doctor will check the position of the needle and then introduce a probe into the disc.
- With the help of laser energy passed through the probe, the surgeon will vaporise some part of the nucleus pulposus.
Finally, the surgeon will stitch up the incisions and place a sterile dressing on the area.
After the surgery, you will be shifted to a postoperative recovery room where your blood pressure, heart rate and respiration will be monitored. Once you are awake, they will shift you to a regular room. You can go home on the same day or may be asked to stay for 1-2 days.
How to care for yourself after discectomy?
Once you return home after the surgery, the following care should be taken:
- As the anaesthesia wears off, you may feel drowsy, confused and unaware of your surroundings, which is normal and will improve slowly.
- You may find your back and hips uncomfortable from spending time in one position.
- You will be advised to take painkillers as needed and as directed by your doctor.
- Bending, lifting any kind of weight or any strenuous activity is strictly not advised for at least two weeks or as recommended by your doctor.
- Driving is not encouraged until a follow-up check by the surgeon or for at least two weeks after the surgery.
- Smoking and the use of alcohol are also not advised.
- You will be provided showering and bathing instructions.
- Wound care: You must ensure that your hands are clean when cleaning the wound. The dressing must be removed and replaced after the area is cleaned with soap and water. Care should be taken to wash the site of the incision daily.
- You will have physiotherapy sessions at four to six weeks after your surgery or based on your condition and progress. Being mobile early after the procedure improves blood circulation and promotes healing.
When to See the Doctor?
You should contact or visit your doctor if you have any of the following conditions:
- The site of the incision appears infected and develops redness, inflammation, oozing or pain.
- You have a body temperature of 101.5°F or more.
- The calf of any of your legs feels sore and has a swelling.
- You develop a tingling sensation like pins and needles or numbness in the legs or groin area.
- You feel a sudden loss of bowel and bladder control.
- You have headaches that are severe and do not go away even after taking painkillers.
What are the possible complications/risks of discectomy?
The risks or complications that arise from a discectomy include the following:
- Increase in back pain.
- Increase in leg pain due to scar tissue around the nerves.
- Injury to the nerve roots during the procedure, which can lead to bowel and bladder dysfunction or muscle weakness.
- Recurrence of disc prolapse.
- Leaking of cerebrospinal fluid due to tearing of the outer covering of the spinal cord. You will need to lie flat for a minimum of 3 days and can have a dull headache for a week.
- Bleeding due to damage to the blood vessels near the spine.
- Infections of the spine or in the disc space.
- Need for further surgeries such as revision discectomy or injections in the spine.
The risks from laser discectomy include the following:
- Infection in the disc
- Injury due to laser
- Pooling of blood under the skin
- Lateral stenosis
- Rupturing of the disc
- Nerve blockage for a short duration
When to follow up with your doctor after a discectomy?
You should schedule a follow-up meeting with your doctor in two weeks after your surgery.
Disclaimer: The above information is provided purely from an educational point of view and is in no way a substitute for medical advice by a qualified doctor.
Surgery Cost In Your City
References
- North American Spine Society [Internet]. Illinois. US; Lumbar (Open) Microscopic Discectomy
- Sharrak S, Al Khalili Y. Cervical Disc Herniation. [Updated 2020 Mar 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Dydyk AM, Ngnitewe Massa R, Mesfin FB. Disc Herniation. [Updated 2020 Apr 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan
- Schoenfeld AJ, Weiner BK. Treatment of lumbar disc herniation: Evidence-based practice. Int J Gen Med. 2010;3:209‐214. Published 2010 Jul 21. PMID: 20689695.
- Sabnis AB, Diwan AD. The timing of surgery in lumbar disc prolapse: A systematic review. Indian J Orthop. 2014;48(2):127‐135. PMID: 24741132.
- Blamoutier A. Surgical discectomy for lumbar disc herniation: surgical techniques. Orthop Traumatol Surg Res. 2013;99(1 Suppl):S187‐S196. PMID: 23352565.
- Wai E, Roffey D, Tricco A,Dagenais S. Evidence-Based Management of Low Back Pain. Elsevier. 2012. Pp:403-421.
- Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976). 2005;30(8):927‐935. PMID: 15834338.
- Resnick DK, Choudhri TF, Dailey AT, et al. Guidelines for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2005;2(6):673‐678. PMID: 16028736.
- Ryang YM, Oertel MF, Mayfrank L, Gilsbach JM, Rohde V. Standard open microdiscectomy versus minimal access trocar microdiscectomy: results of a prospective randomized study. Neurosurgery. 2008;62(1):174‐182. PMID: 18300905.
- Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296(20):2441‐2450. PMID: 17119140.
- Guys' and Thomas' Hospital [internet]: NHS Foundation Trust. National Health Service. U.K.; Lumbar discectomy
- Kambin P; NASS. Arthroscopic microdiscectomy. Spine J. 2003;3(3 Suppl):60S‐64S. PMID: 14589219.