Summary
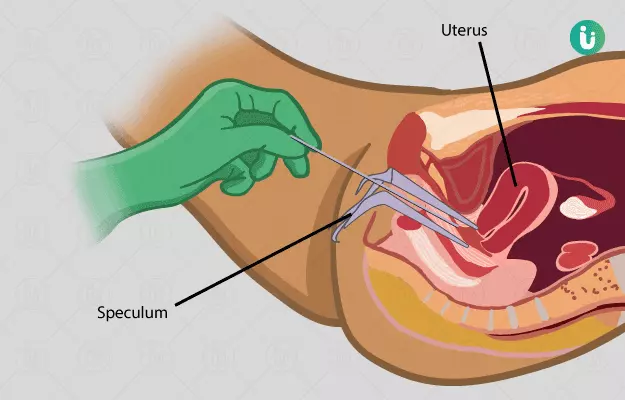
The uterus (womb) is one of the parts of the female reproductive system that undergoes frequent or cyclic changes. It is lined by cells that undergo periodic multiplication in order to support a viable physical environment to grow a baby within. Sometimes, these cellular multiplications may get affected and cause abnormalities or unwanted growth inside the womb. This may affect the ability to conceive. Dilation and curettage is a conventional treatment that has been carried out since ages to manage unwanted pregnancy or abnormal growths within the womb. However, its diagnostic role is questionable as there are newer technologies available to examine the uterus, for example, ultrasound, CT scans, MRI, and so on. Although it is still used as a standard procedure in gynaecological practice, there are various risks and complications associated with it that require careful management of the internal environment of the womb to avoid any damage to the surrounding structures.